Would You Trust a Robot to Perform Your Surgery?
10:39 minutes
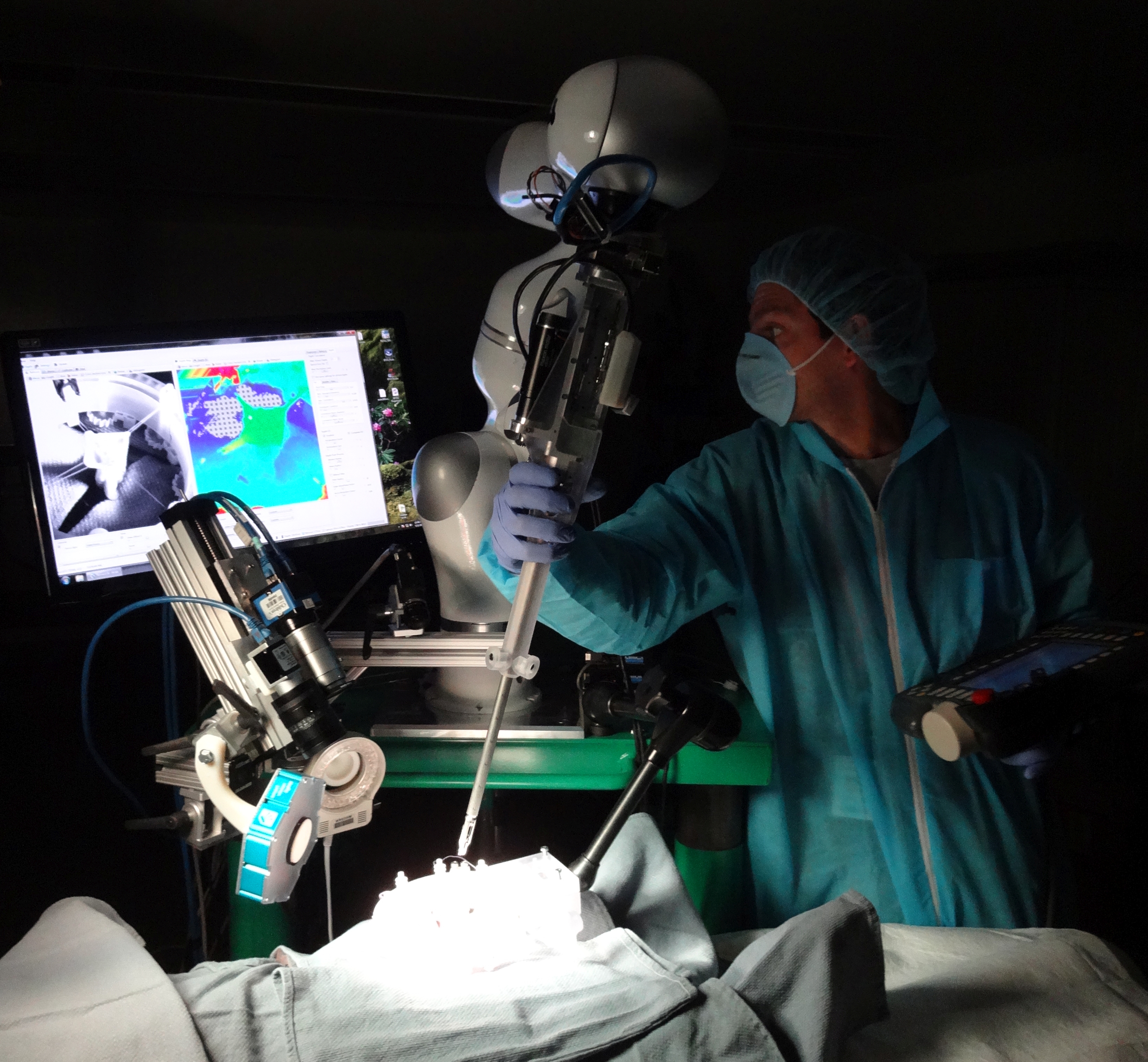
Forget about finding the best surgeon in town. Why not undergo your operation by a robot, which has learned from the best, without the element of human error? Researchers have now developed a robot that can perform sutures and other delicate operations completely autonomously. But would you trust it? Physician Peter Kim and his colleagues recently detailed their invention, which they call the Smart Tissue Autonomous Robot, in Science Translational Medicine. Kim says his goal is to get the robot into hospitals nationwide by keeping the price well below the cost of the surgeon-assisted robots used today.
Peter Kim, MD is Vice President of the Sheikh Zayed Institute for Pediatric Surgical Innovation and Associate Surgeon-in-Chief at the Children’s National Medical Center in Washington, D.C..
IRA FLATOW: Next up, how about a quiz? Just a fun little test on how accepting you are of robots.
Number one– would you trust your life to an autonomous car, let it navigate you through heavy traffic? You know, self-driving car, think about it. Now number two– would you trust your life to an autonomous surgeon? And I’m not talking about a robot that helps a surgeon. I mean a robot that can perform sutures and delicate operations all by itself without the help of a human. You OK with that?
If so, you might have the opportunity to experience surgery at the robotic hands of a machine sometime soon. Because my next guest and his colleagues have developed something they call the Smart Tissue Autonomous Robot, or STAR. And they describe their invention in the journal Science Translational Medicine. And one of the authors is Dr. Peter Kim, vice president of Sheikh Zayed Institute for Pediatric Surgery Surgical Innovation, associate surgeon in chief at the Children’s National Medical Center in DC. Welcome to Science Friday.
PETER KIM: Thank you, Ira, Good afternoon.
IRA FLATOW: So is this right? This robot can operate completely by itself, no surgeon using a joystick or anything like that?
PETER KIM: Well, it is programmed by surgeon. But it can accomplish a complex surgical task, such as anastomosis, which is putting together two tubular structures– whether it be blood vessel or intestine– autonomously as and able, adjust itself, follow, and then provide an optimal functional outcome.
IRA FLATOW: So how do you teach the robot to be a surgeon?
PETER KIM: Well as a surgeon– I’m a pediatric surgeon– I do four things when I do an operation. I spend a little time getting to the problem. I spend most of my time getting rid of the problem and putting it together– and this is like an anastomosis reconstructing. And at the end I spend a little bit of time closing the wound.
So the whole idea is that if you can do the complex, delicate reconstruction part, you can imagine that you can do the entire procedure autonomously. As a surgeon I use my eyes, and my hands, and my mind as in training, and experience, and so on to be able to accomplish a task. And if I can program some of my best ability– a way in which I follow the tissues, and in which I use my hands, and where I make a judgment– into the machine, then one would think that you can accomplish this autonomously.
The purpose is not to simply have a machine do it by itself. But the purpose really is to make the outcomes better. Surgeons have been sewing for hundreds of years, but we really never focused on making the outcomes better. So even when we transitioned from open surgery, to keyhole surgery, to more recently to robotic-assisted surgery, the outcomes have been pretty much the same and complication rates haven’t changed.
And taking anastomosis as an example, if you have a complication– such as a major leak or disruption– your risk of dying from that is three to 10 times higher. So if you have a technology, whether it be autonomous or non-autonomous, and let’s say it improves the chances of having a successful outcome and minimizes complication, why wouldn’t you as an patient or a loved one not wanting to have it.
IRA FLATOW: I guess it’s like a sewing machine can sew better stitches than you could by hand.
PETER KIM: Yes, but it’s a smart one, because it has best sewer’s ideas, and knowledge, and training into it. And at the same time, it adjusts to the changing environment. That’s really the intelligence behind it.
IRA FLATOW: So it gets smarter over time?
PETER KIM: Not this one in particular, this particular generation of it. But over time my idea is that if you can program cumulative experience of all surgeons today and over the history, then any time, if you have a smart machine like this that would have that best practice available to you, then just imagine– anywhere, any place in the world, if you need a particular procedure done, you’ll have a support of history of surgical kind behind you. And that ensures the better outcome, if you will.
IRA FLATOW: So the robotic could then go online and look for the kind of surgery it’s doing and learn how to do it?
PETER KIM: That is in the future. But in this one, just as a proof of concept, we demonstrated that what couldn’t be done before. Because an intestine as a soft tissue is different shades of pink, it’s mobile, it moves, and it’s in the background of other tissue. So it’s very difficult for a machine to know– actually, a machine does not know at all.
All the tools we have to date, including the curtain robotic surgery, is simply a fancy extension, a motorized extension, of surgeon’s hands and skill set, if you will. So it really doesn’t make it any better than your surgeon. Whereas in this case, by programming better practice into it, it helps surgeon and performs better that way.
IRA FLATOW: So this has been tested against good operating surgeons and found to be better than the surgeon?
PETER KIM: That’s right. So when we did the tests we compared essentially putting together a pig intestine done by this particular machine and against the very experienced, internationally-known, surgeons using open technique– as in using their hands– and minimally invasive– as in keyhole surgery instruments– and then currently available robotic instruments. And at the end we measured the quality of anastomosis, how did the gaps of stitching, and how often they made mistakes. And then ultimately the functional outcome is in whether or not it leaks under pressure and so on. The machine, STAR, performed better, surprisingly.
IRA FLATOW: Yeah. Let’s talk about price, because medicine is all about the money.
PETER KIM: It is.
IRA FLATOW: What do you think the price tag of a machine like this is going to come in at?
PETER KIM: So when you do a minimally invasive, the keyhole surgery, the capital cost these days would run somewhere between $80,000 to $100,000. If you buy a robot, it’s $1.5 to $2 million. The way we envision this is that it will be orders of magnitude lower.
But the real value proposition here is that if you can minimize complication, one complication where your risk of dying from it is three to 10 times higher– that is really priceless. So that’s the value proposition for the society as well as the health care system, in addition to making the capital cost of the machine much lower.
Our ideal of robotic surgery is not that the whole thing should be done by a robot from beginning to end, which is the current paradigm, and then robot simply repeats what surgeon does. But robot should come in a time and a place where it does its function best, and then put it away, and then rest of it can be done by human beings.
IRA FLATOW: This is Science Friday from PRI, Public Radio International. I’m Ira Flatow talking with Dr. Peter Kim about new autonomous robotic surgery.
Give me an example. I hear what you’re saying. You’re saying we’re not trying to replace all surgeons.
PETER KIM: No.
IRA FLATOW: We’re trying to replace them where the robot would do something better.
PETER KIM: That’s right.
IRA FLATOW: Give me an example of where you’d use one.
PETER KIM: So they common example would be– we talked about anastomosis– let’s take a hysterectomy, which is relatively commonly performed procedure in this country. I didn’t realize until last year that there are 600,000 hysterectomies done in this country. At the end, you still have to close that little hole. And because it’s way down and deep in a pelvis, the gynecologist, if you will, spend a long time trying to put a handful of sutures in there. And the leakage rate is fairly significant.
Or another example would be, for hernias. And if there’s a weakness in your wall, oftentimes people put up a patch there, almost very much like a carpenter trying to patch up a little hole. And when you put those little sutures around the patch, it is almost like painting the ceiling of the Sistine Chapel– it’s very awkward and so on. When you have an autonomous machine, intelligent machine like this, it can help your surgeon to do that when that task is at hand.
IRA FLATOW: You tested the machine’s ability to stitch two tubular structures together, right?
PETER KIM: That’s correct.
IRA FLATOW: Can it do any surgery or is it more of a one-trick pony for tubular?
PETER KIM: It does linear things. So it is specifically designed to test the anastomosis suturing task. But again, that’s just the proof of concept. Whole idea here is that if you can add intelligence to the current surgical tools and then give it a little bit of autonomy, as in provide a best surgical practice that’s programmed into it, and with the vision technology we have, this will certainly help to minimize the potential complications and then have a better outcome.
IRA FLATOW: Does it need special eyes to work?
PETER KIM: It does have special eyes.
IRA FLATOW: How does it see?
PETER KIM: Well, up until now we’ve always relied on human eyes, human visual spectrum. And including current laparoscopic ones, we’ve focused on more definition, and seeing it brighter, and so on. Whereas this one in particular has what we call 3D quantitative imaging. So it informs the machine where things are in three dimensional space. And we added a little bit of near infrared vision, which is similar to a night vision technology, so that it knows exactly where the targets are. And then it can manipulate the tools and a sub-millimeter accuracy. So that’s really the vision that enables the machine to see better.
And then our goal– we’re working on other sorts of vision technology that will enable the machine and the surgeons to see much better than what human beings would otherwise.
IRA FLATOW: When do you think you get FDA approval for your machine?
[LAUGHTER]
PETER KIM: It will take a few years. But having said that, when we chose some of the components of this technology, we chose ones that are already in clinical practice.
IRA FLATOW: Very smart, very smart.
PETER KIM: So we’re not reinventing the wheel. Very much like an iPhone as an example, the mobile phone, because everything that’s in there is nothing newly invented, but it’s the combination of things that enables it as a mobile platform. The same here– we modified tools and adapted it, we add some new sensors into it. The vision technology, again, is each individual ones are currently used and approved. And then obviously really the smart part is the adding intelligence to the machine.
IRA FLATOW: Well, good luck to you, Dr. Kim.
PETER KIM: Thank you so much.
IRA FLATOW: Thank you for joining us. Dr. Peter Kim, vice president for the Sheikh Zayed Institute for Pediatric Surgical innovation and associate surgeon in chief at Children’s National Medical Center in DC.
Copyright © 2016 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of ScienceFriday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies.
Christopher Intagliata was Science Friday’s senior producer. He once served as a prop in an optical illusion and speaks passable Ira Flatowese.