Forecasting The Future Of Pandemics—In 1994
34:06 minutes
 Since we first went on-air in 1991, Science Friday has brought you news and expert perspectives on the microbes that threaten us—from emerging diseases like AIDS and SARS, to old foes like tuberculosis and plague. In December of 1994, two public health experts took to SciFri’s airwaves to address some disturbing trends in global public health: rising antibiotic resistance, overlooked and underfunded public health infrastructure, and a frightening resurgence of old diseases we thought we’d beat. The guests were Laurie Garrett, then a health and science writer for Newsday and author of the book The Coming Plague (and now senior fellow for health at the Council on Foreign Relations), and Stephen Ostroff, then the associate director of epidemiological sciences at the CDC (and now former acting commissioner of the FDA).
Since we first went on-air in 1991, Science Friday has brought you news and expert perspectives on the microbes that threaten us—from emerging diseases like AIDS and SARS, to old foes like tuberculosis and plague. In December of 1994, two public health experts took to SciFri’s airwaves to address some disturbing trends in global public health: rising antibiotic resistance, overlooked and underfunded public health infrastructure, and a frightening resurgence of old diseases we thought we’d beat. The guests were Laurie Garrett, then a health and science writer for Newsday and author of the book The Coming Plague (and now senior fellow for health at the Council on Foreign Relations), and Stephen Ostroff, then the associate director of epidemiological sciences at the CDC (and now former acting commissioner of the FDA).
With Science Friday celebrating its 25th year in 2016, we’ve reconvened our expert panel to weigh in: What’s changed in the era of Zika and Ebola? And what challenges do we face as we contemplate the next 22 years in pandemics?
Plus, we follow up on last week’s discussion of global El Niño. You asked: What effect is El Niño having on health in Hawaii? This week, Hawaii Public Radio reporter Molly Solomon joins us to share the latest on the state’s dengue outbreak.
Laurie Garrett is a journalist and author with the Anthropos Initiative in New York, New York.
Stephen Ostroff, M.D. is former acting commissioner of the U.S. Food and Drug Administration, based in Silver Spring, Maryland.
Molly Solomon is a general assignment reporter for Hawaii Public Radio in Honolulu, Hawaii.
IRA FLATOW: This is Science Friday. I’m Ira Flatow. New cases of the Zika virus have become so common that you’re hardly hearing anything breaking news about them. We’re having new cases every day. Every week, there’s a new question. Can it be transmitted by sex? What’s the link to microcephaly? What can the US expect with mosquito season around the corner?
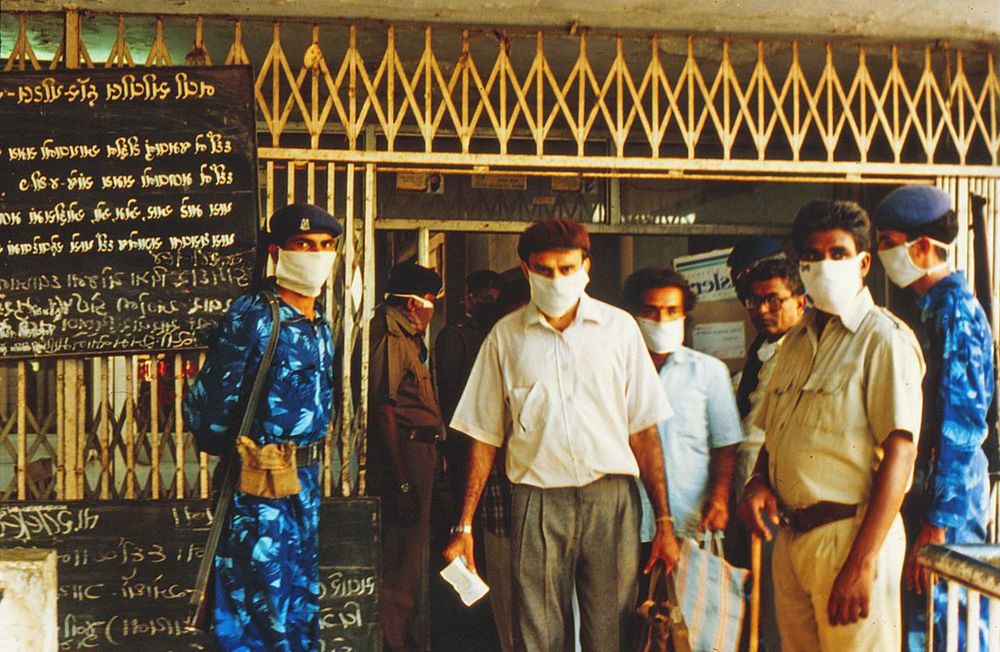
But back in December of 1994, the headlines were a little bit different. Instead of Zika, think Hantavirus. Remember that one? It struck the Southwest Four Corners in 1993, infecting dozens before cropping up again in New York in ’94. And 1994 also brought plague, the poster child for infectious diseases. An outbreak in India back then killed 56, raising disturbing questions about our ability to combat diseases we thought we had already licked. The diseases changed, but the questions stay the same.
How do we detect outbreaks faster, develop cures– get them to the people who need them the most? Well, back in 1994, two public health experts came on our show to talk just about that. Laurie Garrett was a health and science reporter for Newsday back then. She was out with a new book The Coming Plague. Our second guest, Dr. Stephen Ostroff, then the CDC’S associate director for epidemiological sciences.
Well, with Science Friday celebrating our 25th year this year, we decided to check back in with our guests. What’s changed in the era of Zika and Ebola? So here they are. Laurie Garrett is the senior fellow for global health at the Council on Foreign Relations in New York. She’s here in our New York studio. Always good to have you back, Laurie.
LAURIE GARRETT: Hi, Ira.
IRA FLATOW: Steven Ostroff– Dr. Ostroff is the former acting commissioner for the FDA. I think he was that till yesterday. He joins us today from Washington welcome back, Dr. Ostroff.
DR. STEPHEN OSTROFF: It’s a pleasure to be with you.
IRA FLATOW: Laurie, I’m going to start with you. Looking back over the last 22 years, are you more struck by what’s changed or by what’s stayed the same?
LAURIE GARRETT: Well, I’m struck by what’s changed in one way and what’s stayed the same or gotten worse in another way. What has changed very dramatically is back in 1994 when Steve and I were on this show and when my book came out, it was a controversial premise– the notion that we had not defeated infectious diseases– that they would surge back– that we were not comfortably in the age of just thinking about cancer and heart disease. That has completely changed. And I think now from the highest levels of government right on down, people realize that we had a major hubris problem back in the day and that the microbes are constantly mutating and posing new challenges.
What frustrates me is that we continue to have with every single outbreak– every single portent on the horizon such as losing the efficacy of antibiotics– we continue to have two trends that just constantly re-emerge. One is government saying let’s kick that down the road. We’ll deal with it when it’s in our face. But we don’t really want to put time, energy, and money into it before a catastrophe.
And the second is that when catastrophe hits, the public goes berserk. And every single time the conspiracy theorists come out of the walls. The people who claim government doesn’t know what it’s doing. And the public health officials like Steve Ostroff have to fight the exact same battles in terms of public opinion and mobilizing whacko politicians over and over. And that’s true in every country in the world. That’s not a uniquely American sad phenomenon.
IRA FLATOW: Let me go back to 1994. Let me go back to a piece of tape of Dr. Ostroff back in ’94. You warned us in no uncertain terms that antibiotic resistance was going to be a big problem.
DR. STEPHEN OSTROFF: I think that we have unfortunately squandered a wonderfully golden gift which was given to us 50 or 60 years ago. And that was the gift of antibiotics. And I think many of us fear as we approach the end of the 20th century that we’re getting into a situation where we went from the pre-antibiotic era, to the antibiotic era, to the post-antibiotic era.
IRA FLATOW: Dr. Ostroff, are we in the post-antibiotic era?
DR. STEPHEN OSTROFF: Well, I was certainly fascinated to hear that particular quote again, because when I said that, it was at a time where I don’t think that there was a lot of attention being paid to the growing problems that we were seeing with antibiotic resistance. And if my memory serves me correctly, I know that several of the federal agencies a couple of years later put out a report about things that could be done to address the problem of antimicrobial resistance.
And in fact, Ira, this was at the time I was at CDC. And I know that we updated that report a couple of years later. But the topic itself didn’t really get a lot of attention or a lot of traction. But I think one of the things that has changed in recent years, particularly in the last couple of years, is the recognition that this is a really serious and growing problem and that it has gotten to what I would refer to as the tipping point where we really do have to pay attention to this. We have to devote significant resources to the problem.
And we have to do something to reverse the trends that we’ve seen. And I think that even at the highest levels of government, you hear now President Obama talking about this. You hear leaders in Europe and the World Health Organization talking about that particular topic. So I’m very hopeful that with this recognition that there really is the potential with appropriate investments of resources to be able to do something about this.
IRA FLATOW: But it’s not the government that’s going to make the antibiotics. Right, Laurie? It’s the corporations that are going to make them.
LAURIE GARRETT: I want to share Steve’s optimism. But we have two plasmids in circulation. A plasmid is a little package of DNA. We have two in circulation that are now showing up all over the world in all kinds of different bacterial populations that confer combined universal antibiotic resistance. They render everything useless for bacterial attack. And when the first one emerged about four years ago in New Delhi, people said, well, we have one case imported to the UK. And the rest is in India.
We’ve got time for the industry to get mobilized and for somebody to figure out what to do. And that’s now, as far as I know, everywhere in the world. It’s called NDM-1. We have another one that surfaced just recently in China. And it’s already in 30 countries. The problem is that the industry wants a home run with high profit potential immediately. What they’re not interested in is replacing the old stalwarts, or streamlining penicillin, or coming up with better ways to package the off-patent drugs.
And there aren’t a lot of new targets that anybody’s found that seem to make a lot of sense. The other problem is that every new significantly new drug is exponentially more expensive than whatever predated it. And we’re getting to the point where effectively we have untreatable bacterial infection for economic reasons already in much of the world, because they can’t afford the new drugs, even if they do come out.
IRA FLATOW: Let’s move on to another bit of tape from 1994. Laurie, when you warned us in ’94 about cost cutting.
LAURIE GARRETT: We have had enormous budget cutting atmosphere in the United States. And some of the things that have been devastated have been those routine public health programs like mosquito control, rat control. And these programs have taken huge slashes according to the CDC’s own studies at the local level. At the state level and municipal level, we are in very bad shape in this country. And we should not be complacent. We should not sit back and think, oh, yeah, we have this great body. And if anything happens, they’re going to move in and take care of the situation. That’s not the state of affairs at this time.
IRA FLATOW: What is the state of affairs this time?
LAURIE GARRETT: Oh, goodness. A couple things happened after that that have, in some ways, made matters much worse. And Steve was part of one of them. We had a little problem called anthrax mailings in 2001. And Steve was leading investigations here in New York. And one of the things that happened after that was a kind of securitization under the Bush administration, Bush W., of the CDC and public health all across the country with a huge skewing of expenditures and personnel towards being ready for anthrax, being ready for biological weapons, blah, blah, blah– running drills.
Every hospital in the country had– here’s the secret bioterrorist agent been released. Be prepared. Demonstrate you can move the patients around. And in many states, many places I went, people bemoaned that in order to accommodate these federal mandates, they eliminated their mosquito control program. They eliminated their mammography and breast cancer awareness program. They eliminated their STDs, Sexually Transmitted Disease program. And then at the local level– you have to remember that even though we have this great CDC, public health in America really is a local function.
IRA FLATOW: Yeah, first responders.
LAURIE GARRETT: First responders. And at the local level, it’s a big ouch.
IRA FLATOW: All right. Stephen would you agree that–
DR. STEPHEN OSTROFF: Well, I have to say I think that Laurie has really hit the nail on the head, as she so often does. One of the things that it’s worth pointing out is that in between my latest job and when I left the CDC in 2005, I was actually working at the state level in Pennsylvania for a number of years. And so I’ve seen both sides of the equation. And while Laurie’s correct that there are now considerably more resources available than there were back in 1994, we still suffer from a phenomenon of seeing large amounts of resources devoted to a problem while it’s very highly visible and everyone is paying attention to it.
But the difficulty tends to be sustaining those resources over time. And so as Laurie mentioned, with the anthrax episode, there was a large infusion of resources. We saw the same phenomenon when the pandemic H1N1 came along in 2009. For a while, we saw it with West Nile. And of course, the same occurred with Ebola.
But the difficulty is once people’s attention tends to fade and they turn to other problems, the resources tend to dwindle down as well. And one of the important lessons that you learn is that the same people who are dealing with each of those– for each of those problems, it’s the same people that are on the front lines trying to address them. And the important issue is making sure that we sustain the infrastructure that’s necessary all the time because as you know, these problems tend to come up over and over again. And I think that they will continue to do so.
LAURIE GARRETT: Well, I’ll tell you one that’s coming right now. People tend to think– you hear the phrase mosquito abatement. And it sounds like [SNORING] boring. But these are the folks that actually have the skill set to how to not poison you, not put DDT on your front lawn, but stop those mosquitoes. We’ve got Zika. It’s lapping at our shores.
We’re in winter now . But as we go to summer, we’re going to see all the proper populations of mosquitoes emerging across the southern United States. And you’re going to find out that mosquito abatement, if it works, requires people that are there year after year after year. They have a skill set. You can’t just pull a kid out of high school and say, go out and spray the bushes. And we will see which states have maintained mosquito abatement personnel and programs and which have done cutbacks. And then we’ll pay a price with Zika as we get into summer.
IRA FLATOW: So we’re just playing sort of a whack-a-mole all the time.
LAURIE GARRETT: Absolutely. That’s the story of public health– whack-a-mole.
DR. STEPHEN OSTROFF: Yeah, I have to say, because West Nile was something I was very heavily involved in when it first arrived on our shores in 1999– and we did certainly have an infusion of resources over the next year or two to be able to address the infrastructure, even to monitor where the mosquitoes were, let alone have programs to be able to do mitigation.
And over the next several years, those resources dwindled considerably. I wrote an article after an outbreak that had occurred in Dallas, Texas a couple of years ago. And the title of that article was West Nile: Forgotten but Not Gone. And so I think one of the unfortunate consequences is that we’re reaping the results of allowing that infrastructure that was put in place for West Nile to have deteriorated. And now we need it again.
IRA FLATOW: Let’s see if we can get some callers to call in– 844-724-8255 is our number. If you’d like to tweet us, you can also tweet us @scifri here on Science Friday talking with the Laurie Garrett and Stephen Ostroff from Science Friday from PRI, Public Radio International.
I’m Ira Flatow. Let’s go back to the wayback machine and get another clip. This was a caller named Jesus who asked us very prescient question.
JESUS: Does the CDC or the military have any plans for any sort of emergency that may develop, particularly with some of these viruses, including Ebola, which could be potentially quite nasty?
IRA FLATOW: Talking about Ebola.
LAURIE GARRETT: Yeah. That’s a really prescient question and one that I’ve devoted most of my adult life to trying to deal with. What happened was when Ebola broke out about three or four months after we taped this, we were on the air in 1995 in Kikwit. And I went to Kiwit and was in the middle of the epidemic for most of the duration of it and came back and found that the government was quite disturbed. And everybody was suddenly revved up. And we need a plan.
And then, of course, they forgot about we need a plan until after anthrax. Then they beefed up– we need a plan again. That one was very biased towards bioterrorism and was forgotten after a while. And then in 2005 after we’d had the SARS epidemic around the world in 31 nations and then H1N1, as Steve referred to, the swine flu, was looming in 2009. But 2005 was the turning point because a previously obscure bird flu mutated called H5N1.
IRA FLATOW: I remember that.
LAURIE GARRETT: And suddenly had the capacity to infect a wider range of birds and came into Europe and down into Northern Africa. And the Bush Administration became very distressed. I found myself briefing the National Security Council, the State Department, CIA. What are we going to do about this? And so the Bush Administration put together a very, very detailed pandemic influenza plan. And for the first time, it was a plan that really linked to the international picture.
So it didn’t imagine fortress America being able to, I guess as Donald Trump would say, build giant walls to keep microbes out. Or as Governor Christie would say, let’s just quarantine them all. It was a plan that said our security is linked to what’s going on everywhere in the world. And we have to help the poor countries of the world to build up their capacity to identify and respond to disease.
Now, every government since has had permutations. And currently the Obama Administration has the global health security initiative trying to bring all the countries in the world up to speed. And we’ll see if the Republicans will continue to support it.
IRA FLATOW: My guests are Laurie Garrett, senior fellow for global health at the Council on Foreign Relations– Stephen Ostroff, former acting commissioner at the FDA. Our number, if you’d like to call us, 844-74-8255. We’re going to take a break and then come back and talk lots more about it. So stay with us. We’ll be right back.
This is Science Friday. I’m Ira Flatow. We’re talking this hour about pandemics and public health. What can past outbreaks teach us about protecting ourselves today? My guests are Laurie Garrett and Stephen Ostroff. We’re going to continue talking about the epidemic and dip into our tapes from back in 1994. But first, I want to follow up on a conversation you may have heard on the show last week about the global effects of El Nino. Caller Hans in Sturgeon Bay, Wisconsin asked us this question.
HANS: So it’s not really a health question. But I was just curious about given where El Nino tends to start in the Pacific Ocean, if it has any sort of effect on the Hawaiian Islands?
IRA FLATOW: Well, it turns out it was a health question. We didn’t have an answer for Hans last week. But joining me now is Molly Solomon, a reporter at Hawaii Public Radio. And she’s going to bring us up to date on the latest dengue outbreak in the state– Hawaii’s third dengue outbreak in 15 years. Molly, thanks for joining us.
MOLLY SOLOMON: Thanks, Ira, happy to be here.
IRA FLATOW: How many cases are we talking about now?
MOLLY SOLOMON: So I just checked and currently, as of yesterday afternoon, there are 260 total cases of dengue fever in Hawaii right now. Right now they’re all on Hawaii Island. That’s the Big Island of Hawaii. And about 90% of those are folks that live there, residents. About 25 or so are visitors that have come to the islands on vacation. But it has slowed in recent days or the last week or so. We’ve only had one case reported since last Friday.
IRA FLATOW: You know, if there were 260 cases in any other state of the Union, it’d be leading the news. We don’t hear a thing about it here on the mainland.
MOLLY SOLOMON: That’s right.
IRA FLATOW: It’s unbelievable.
MOLLY SOLOMON: And I’m sure a lot of folks here in what are a little disappointed that others don’t know about the dengue outbreak that is going on right now.
IRA FLATOW: Do we know how it arrived in Hawaii?
MOLLY SOLOMON: We do. The outbreak that we’re currently dealing with– it came from someone that was infected in another country. They came back to the islands. They probably didn’t know that they had dengue fever. And then a mosquito bit them. And that mosquito then became infected with dengue fever and went on to bite other people and passing on the disease from there. And this actually happened in September of last year and snowballed throughout the later end of the year and is still going on right now.
IRA FLATOW: And how has the state responded?
MOLLY SOLOMON: The state is doing a couple things. I think a lot of people, public opinion, felt that they were a little slow at first. But they have since ramped up efforts. They’ve been spraying at homes and yards where folks that have been contaminated with the virus. They’ve sprayed in the areas where they’ve been seen as high risk in Kailua-Kona. They shut down two beaches as well as a popular area called Waipio Valley.
And I think the big problem with Hawaii Island is that it is one of the more rural islands. So you’re dealing with a place that is very tropical. There’s a lot of plants and areas that would be prime breeding sites for mosquitoes. So I think it’s difficult for the state to deal with this, especially, I think, because of something that you actually were talking about earlier is the cuts to vector control programs in local communities in different states. It’s something that Hawaii has experienced.
Back in 2009, they had cuts to their state’s vector control program. And it actually got gutted practically in half. So there are only 25 people versus 56, which is what they used to have. I think that’s had a pretty big effect in that the folks that are working to spray these areas notify the public. They’ve been stretched pretty thin. They’ve been working seven-day weeks trying to get the information out.
IRA FLATOW: Yeah, Laurie, you were briefing congressional staffers just this week.
LAURIE GARRETT: Yes.
IRA FLATOW: They had no idea.
LAURIE GARRETT: They didn’t know anything about it. They didn’t know that there was a dengue outbreak in Hawaii. And I was saying to them pay attention, because the reason Hawaii has had three rounds of dengue is because of the introduction of Asian mosquitoes to the Hawaiian Islands not native to the islands Aedes albopictus.
Now we’ve had Aedes aegypti introduced to North America via slavery back 300 years ago. And then Aedes albopictus was introduced via the trade in recyclable tires. And the mosquitoes lay their larva in the tires in Malaysia, and they ended up in Brazil. Well, we’ve been warning over and over again. And I’m sure Steve Ostroff can tell wild stories about how hard it’s been to get politicians to focus on this.
But here’s these dangerous mosquitoes. All you need, as happened in Hawaii, is one person showing up at the right time, the right temperature, the right weather conditions, getting bit. That mosquito goes and bites 10 other people, and boom, you start to have an outbreak. And so I was saying to the congressional staffers, we will have local transmission of Zika. It will happen. So start looking now. What do your mosquito abatement programs look like?
IRA FLATOW: Well, Molly, thank you very much for you’re letting the rest of the country know about what’s going on in Hawaii.
MOLLY SOLOMON: Happy to do so. Thanks for having me on, Ira.
IRA FLATOW: You’re very welcome. Molly Solomon is a reporter at the Hawaii Public Radio. And she joined us today from San Francisco. Moving on, Dr. Ostroff, in 1994 going back, you could confidently say this. You could say this about vaccines.
DR. STEPHEN OSTROFF: When you talk about some of the childhood vaccines, I think that we’ve done a wonderful job in making sure that the children who need these vaccines actually get them.
IRA FLATOW: Would you ever have predicted, Dr. Ostroff, the resistance we’re seeing today to childhood vaccines in this country?
DR. STEPHEN OSTROFF: Well, I think that’s a really interesting question. And I think that there has always been concerns about vaccines. I think that we have such better information and such better science to refute most of those concerns. What I will say is that we still have superb vaccination levels across the entire population in many of our children because of available programs. But what we don’t have is we don’t have consistent levels of vaccination throughout the country.
And so we’re faced with circumstances where there are pockets of under-immunization. And those pockets of under-immunization unfortunately leave many other people at risk of acquiring diseases where we thought we wouldn’t see problems with them. And I think the poster child for this is the problems we’ve seen with measles in the past year or two where back in 2000, measles was considered to have been eliminated from the Western Hemisphere.
And yet, we continue to have problems. And those problems occur because in the other part of the world, measles is not eliminated. And so all that has to happen is somebody either travels to that area or somebody from those areas traveled to the United States and find those individuals who are under-immunized. And you spark these problems. And so I think that it is something that we have to continue to pay very close attention to because these problems, I think, will continue to occur unless we have better ways of being able to get those who need to be immunized, immunized.
IRA FLATOW: Laurie, here here’s something that you said about vaccines back in ’94.
LAURIE GARRETT: At this time in the world, there is no financial incentive whatsoever to vaccine manufacturers to make a vaccine that targets a microbe that primarily affects the developing world. At this time, there is every disincentive imaginable. They will not make any money off of it.
IRA FLATOW: Now, don’t you have some good news to tell us?
LAURIE GARRETT: Well, yeah, a couple things have happened. One is the creation of GAVI, the Global Alliance of Vaccinators and Immunizers, which now has billions of dollars to spend every year thanks in large part to Bill Gates and to David Cameron, the prime minister of the UK. This entity does a couple of things. One, it purchases massive quantities of vaccines and gets them to poor countries. That creates an incentive to industry. They know someone will buy the product. And so they continue to make them.
And then just recently, when the Ebola vaccine was developed on site in the epidemic in West Africa, GAVI said to industry, we will put up a pot of gold right here if you go out and make this vaccine and build a stockpile and store it under proper conditions so that it will last for many, many years in case we need it in the future. And that shows that if you create the right incentive systems, you can have breakthroughs.
The problem is that it still is the case that without special money like I was just describing, industry wants a home run in the pocketbook. And that means targeting Americans and Europeans basically. And that limits a lot of the range of possibilities. Now, two big success stories of late– one, which was highly controversial in this country and continues to be controversial in certain political sectors of our society– the human papillomavirus vaccine, or HPV vaccine, just announced in studies published this week– 64% reduction in girls and women diagnosed with cervical carcinoma or pre-cervical carcinoma because of that vaccine. Fantastic! The dividends down the road not just in lives saved, but in cost to society for treatment and care of cancer. Fantastic!
And then we just had published this week in Science Magazine a breakthrough study looking at two survivors from the 1995 Ebola epidemic in Kikwit, the one I was in before I was also in the 2014 epidemic. And they found in these two survivors that these individuals all these years later have extremely high levels of effective antibodies in their body that could be administered to rhesus monkeys and then inject Ebola live virus directly into those monkeys and every one of the monkeys that was immunized survived and cleared the virus completely.
IRA FLATOW: Amazing!
LAURIE GARRETT: This is a spectacularly successful possibility. And if industry can be incentivized to develop both treatment and vaccine based on this, we could almost effectively say that Ebola is rendered a development issue, not a medical issue.
IRA FLATOW: And as far as the link to Zika virus to microcephaly, is there any news on that?
LAURIE GARRETT: Yes, there is. And that was just published today at 2:00 PM on PLOS. It is the discovery jointly by Yale University and a team in Brazil of a young woman who was pregnant and had a sonogram that showed her baby at 18 weeks was already malformed. They tracked this child all the way to stillbirth at 32 weeks then conducted immediate autopsy. And they were able to demonstrate the fetus had microcephaly, had profound neurological issues. And they’ve discovered active virus in the child’s brain tissue, central nervous system, and some other tissues in the body. I think that’s a pretty big home run.
IRA FLATOW: I’m Ira Flatow. This is Science Friday from PRI, Public Radio International, talking with Laurie Garrett and Stephen Ostroff. A few minutes left, Stephen, are you hopeful? More hopeful than you were 22 years ago?
DR. STEPHEN OSTROFF: Well, it’s a really interesting question. In the whole topic of emerging infectious disease, my point of reference is a report that was issued by the Institute of Medicine of the National Academy of Sciences actually in 1992. And it was the basis for some of the recommendations that were made by the CDC a year or two later about how to address these. But in that ’92 report, there were six factors that were mentioned very specifically as being sort of the root causes of emerging diseases. And one of them was changing human demographics.
One of them had to do with technologic changes that we ourselves do. Another one was changes in the environment. The fourth was travel and human movement. The fifth was microbial adaptation, and the sixth was failure to implement tried and true public health measures. And if you think about many of those factors, they are absolutely just as relevant today as they were back in 1992. And if you think about those trends in those various factors, many of them have gone in the direction that favor the microbes.
And so I don’t think that we should have the same levels of hubris that you started out the segment with about the end of the era of infectious diseases, because I do think that we will continue to see events of the type that we’ve seen over the last few years. And that’s why it is so critically important to keep the infrastructure in place so that we can address these. One of my favorite quotes is that if you think prevention is hard, try response. And so we’d much rather be in a position where we can prevent some of these things from happening rather than just being in this continuous fire drill way of dealing with these.
IRA FLATOW: Well, this being an election year, how do you raise this issue? How do you get it into the conversation?
LAURIE GARRETT: Well, unfortunately, it’s already been raised, but in the wrong ways. Chris Christie just before he actually stepped out of the campaign said, if asked, he would be happy to enforce quarantine to stop Zika, just as he did by isolating Kaci Hickox, the nurse who returned from Sierra Leone and was negative for Ebola. But he kept her for 80 hours in a tent on the tarmac in Newark, New Jersey.
We’ve already had Rand Paul. And all the candidates that are still on the GOP side have addressed the possibility of refusing vaccines– the notion that it’s an individual right to say, no, I don’t want to get vaccinated. I don’t want to vaccinate my children. But I do want them to go to school with your kids and possibly give them measles. And we unfortunately see these issues come in in the wrong way consistently in campaigns. And this is true not just this year, but every presidential round. They enter more in a reactive way than what would–
IRA FLATOW: So what would be the right way?
LAURIE GARRETT: Well, the right way is to talk about what is the nature of the health infrastructure and also, say, to de-link– de-link emerging diseases from immigration. There’s no evidence at all that we face diseases because of immigrants. We face diseases because of global trade, travel, and globalization, which are essential to our economy. We can’t suddenly say we won’t go overseas anymore. We have to figure out much more creative ways and ways that involve international solidarity instead of international divisiveness and hatred to combat shared risk and provide shared benefits.
And that’s the real challenge point we’re at right now is that much of the world doesn’t trust us. They don’t trust Americans. They think we’re a bunch of lying scumbags on this issue. I guarantee you I hear it over and over again, because they will say, every time a new disease occurs, you guys get all the vaccines. You guys get all the drugs. And then you come to us and say, build an infrastructure to protect. You just want yourselves protected. You don’t care if we die.
IRA FLATOW: You’ve got the last word on that, Laurie Garrett, senior fellow for global health at the Council on Foreign Relations. You’ll notice she does not mince her words when she speaks. Stephen Ostroff is the former acting commissioner of the FDA. I want to thank you both for joining me today.
DR. STEPHEN OSTROFF: It was terrific to be with you.
IRA FLATOW: We’ll check back in 2038. How about that?
LAURIE GARRETT: All right.
IRA FLATOW: All right. Special thanks to–
DR. STEPHEN OSTROFF: We’ll be here.
IRA FLATOW: Special thanks to listener Sheri Gallo who tipped us off to the dengue outbreak in Hawaii. Thanks, Sheri.
Copyright © 2016 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of ScienceFriday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies.
Annie Minoff is a producer for The Journal from Gimlet Media and the Wall Street Journal, and a former co-host and producer of Undiscovered. She also plays the banjo.