Which Came First: The Chicken Or Antibiotic Resistance?
In her new book, Maryn McKenna unspools the misuse of drugs, and chronicles how food animals may have created bacteria more resistant to human medicine.
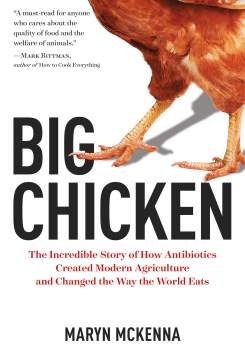
The following is an excerpt of Big Chicken: The Incredible Story of How Antibiotics Created Modern Agriculture and Changed the Way the World Eats, by Maryn McKenna.
For most people, antibiotic resistance is a hidden epidemic, unless they have the misfortune to contract an infection themselves or have a family member or friend unlucky enough to become infected. Drug-resistant infections have no celebrity spokespeople, negligible political support, and few patients’ organizations advocating for them. If we think of resistant infections, we imagine them as something rare, occurring to people unlike us, whoever we are: people who are in nursing homes at the end of their lives, or dealing with the drain of chronic illness, or in intensive-care units after terrible trauma. But resistant infections are a vast and common problem that occur in every part of daily life: to children in day care, athletes playing sports, teens going for piercings, people getting healthy in the gym.
And though common, resistant bacteria are a grave threat and getting worse. They are responsible for at least 700,000 deaths around the world each year: 23,000 in the United States, 25,000 in Europe, more than 63,000 babies in India. Beyond those deaths, bacteria that are resistant to antibiotics cause millions of illnesses — two million annually just in the United States — and cost billions in health care spending, lost wages, and lost national productivity. It is predicted that by 2050, antibiotic resistance will cost the world $100 trillion and will cause a staggering 10 million deaths per year.
Disease organisms have been developing defenses against the antibiotics meant to kill them for as long as antibiotics have existed. Penicillin arrived in the 1940s, and resistance to it swept the world in the 1950s. Tetracycline arrived in 1948, and resistance was nibbling at its effectiveness before the 1950s ended. Erythromycin was discovered in 1952, and erythromycin resistance arrived in 1955. Methicillin, a lab-synthesized relative of penicillin, was developed in 1960 specifically to counter penicillin resistance, yet within a year, staph bacteria developed defenses against it as well, earning the bug the name MRSA, methicillin-resistant Staphylococcus aureus. After MRSA, there were the ESBLs, extended-spectrum beta-lactamases, which defeated not only penicillin and its relatives but also a large family of antibiotics called cephalosporins. And after cephalosporins were undermined, new antibiotics were achieved and lost in turn.
Each time pharmaceutical chemistry produced a new class of antibiotics, with a new molecular shape and a new mode of action, bacteria adapted. In fact, as the decades passed, they seemed to adapt faster than before. Their persistence threatened to inaugurate a post-antibiotic era, in which surgery could be too dangerous to attempt and ordinary health problems — scrapes, tooth extractions, broken limbs — could pose a deadly risk.
[Old ideas may help us fight new superbugs.]
For a long time, it was assumed that the extraordinary unspooling of antibiotic resistance around the world was due only to misuse of the drugs in medicine: to parents begging for the drugs even though their children had viral illnesses that antibiotics could not help; physicians prescribing antibiotics without checking to see whether the drug they chose was a good match; people stopping their prescriptions halfway through the prescribed course because they felt better, or saving some pills for friends without health insurance, or buying antibiotics over the counter, in the many countries where they are available that way, and dosing themselves.
But from the earliest days of the antibiotic era, the drugs have had another, parallel use: in animals that are grown to become food. Eighty percent of the antibiotics sold in the United States and more than half of those sold around the world are used in animals, not in humans. Animals destined to be meat routinely receive antibiotics in their feed and water, and most of those drugs are not given to treat diseases, which is how we use them in people. Instead, antibiotics are given to make food animals put on weight more quickly than they would otherwise, or to protect food animals from illnesses that the crowded conditions of livestock production make them vulnerable to. And nearly two-thirds of the antibiotics that are used for those purposes are compounds that are also used against human illness — which means that when resistance against the farm use of those drugs arises, it undermines the drugs’ usefulness in human medicine as well.
[Michael Pollan says you are what you cook.]
Resistance is a defensive adaptation, an evolutionary strategy that allows bacteria to protect themselves against antibiotics’ power to kill them. It is created by subtle genetic changes that allow organisms to counter antibiotics’ attacks on them, altering their cell walls to keep drug molecules from attaching or penetrating, or forming tiny pumps that eject the drugs after they have entered the cell. What slows the emergence of resistance is using an antibiotic conservatively: at the right dose, for the right length of time, for an organism that will be vulnerable to the drug, and not for any other reason. Most antibiotic use in agriculture violates those rules. Resistant bacteria are the result.
Experimenters began trying the then new miracle drugs in animals almost as soon as antibiotics were achieved in the lab in the 1940s — and concern about that use dates just as far back. From the start, in protests that were downplayed for decades, a few perceptive researchers warned that resistant bacteria would arise in livestock, find a way off farms, and move silently through the wider world. The shortest route off farms is in the meat that animals eventually become: In the year Schiller got sick, 26 percent of the Salmonella found on supermarket chicken by government testing was resistant to at least three separate families of antibiotics. But resistant bacteria also leave farms in manure, in storm runoff, in groundwater, in dust, and via the skin and clothes and microbial hitchhikers of people who work on farms and live there. When those organisms escape, they disperse in a manner that is impossible to track, and they cause illness and alarm far from the farms where they originated.
Excerpted from Big Chicken by Maryn McKenna, published by National Geographic Partners on September 12, 2017. Copyright © 2017 by Maryn McKenna. Available wherever books are sold.
Maryn McKenna is a science writer and columnist for Wired. She’s also the author of Big Chicken: The Incredible Story of How Antibiotics Created Modern Agriculture and Changed the Way the World Eats.