Instead Of A Vaccine For Lyme, How About A Vaccine For Ticks?
When ticks bite us, they release thousands of proteins through their saliva. Could a vaccine for the right ones stop ticks from latching on?

An adult female blacklegged tick (Ixodes scapularis). Credit: CDC/ Division of Vector-Borne Diseases Rickettsial Zoonoses Branch
 Lyme disease is on the rise in the United States, but there’s still no vaccine for it on the market. While that’s frustrating to many, especially those who have experienced long-term effects of the disease, some people who live in prime tick territory say they don’t need it.
Lyme disease is on the rise in the United States, but there’s still no vaccine for it on the market. While that’s frustrating to many, especially those who have experienced long-term effects of the disease, some people who live in prime tick territory say they don’t need it.
“ When you talk to older residents in endemic areas like Block Island or other areas [in the] Northeast, and you ask them if they wanted a Lyme disease vaccine, they would often tell you … ‘Oh, I don’t worry about ticks that much anymore. They don’t seem to bite me,’” says Dr. Erol Fikrig, a professor of medicine and chief of the Section of Infections Diseases at Yale’s School of Medicine.
This phenomenon, called “acquired tick resistance,” occurs when a person’s immune system learns to fight off ticks on its own after repeated bites. Although we only know it happens on a large scale because of scattered stories from tick country, Fikrig’s team is beginning to formalize the research into how it works. He and his colleagues think understanding the mechanisms behind acquired tick resistance could lead to an even better vaccine than one for Lyme: a vaccine against the tick itself.
In a March study, Fikrig and his colleagues designed a tool to investigate how the immune system responds to a vast collection of proteins that a tick releases when it bites. If scientists can identify which ones our immune systems reliably react to, an anti-tick vaccine could be possible.
To infect its host with Lyme disease, a tick typically needs to be feeding for at least 24 hours. Removing the tick in time may help prevent disease transmission, but ticks have evolved a number of ways to make sure you don’t notice them until they’re done with you.
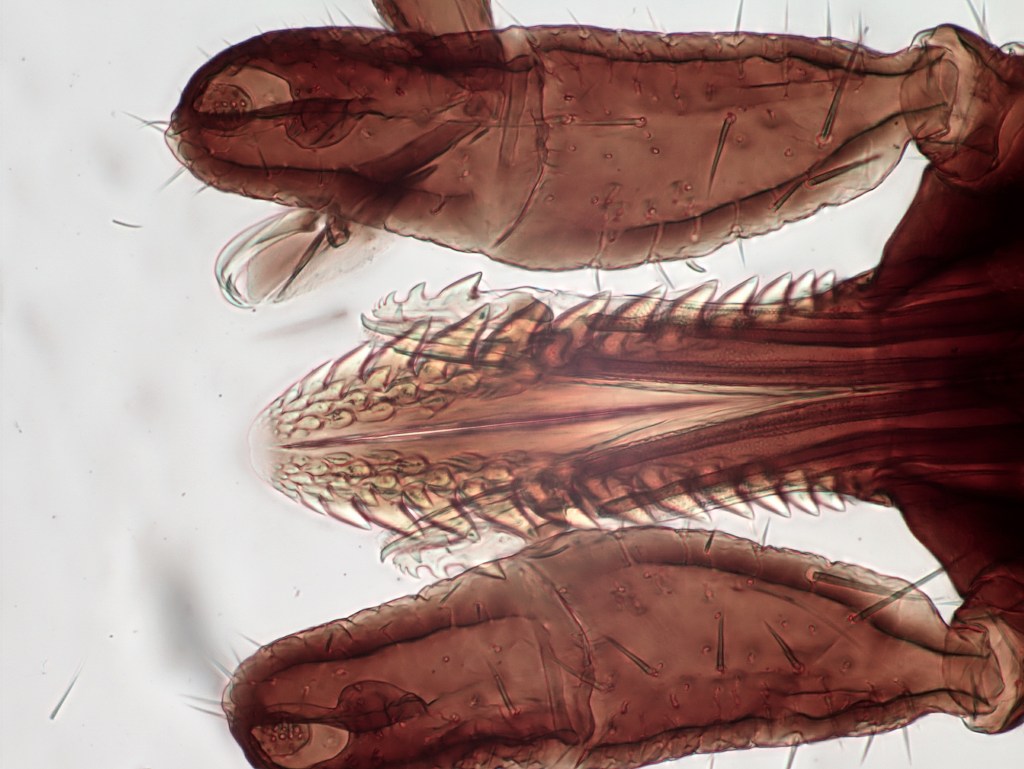
When a tick bites its host, it inserts its jagged needle-like mouthpart, called a hypostome, into the host’s skin. From there, it releases a “pharmacopia” of proteins through its saliva, says Dr. Richard Ostfeld, a disease ecologist at the Cary Institute of Ecosystem Studies in Millbrook, New York. These proteins work like anesthetics, antihistamines, and anticoagulants—making sure the host doesn’t feel the tick’s presence and the blood keeps flowing. Tick saliva also contains “cement proteins,” which help it stay stuck tight to the host while feeding.
The immune systems of people with acquired tick resistance are able to recognize and fight one or more of the proteins the tick secretes when it bites. For Ostfeld, who has acquired tick resistance himself, ticks get “very lightly attached” to his skin, and usually die early in the process of attaching. “I’m killing them rather quickly,” he says.
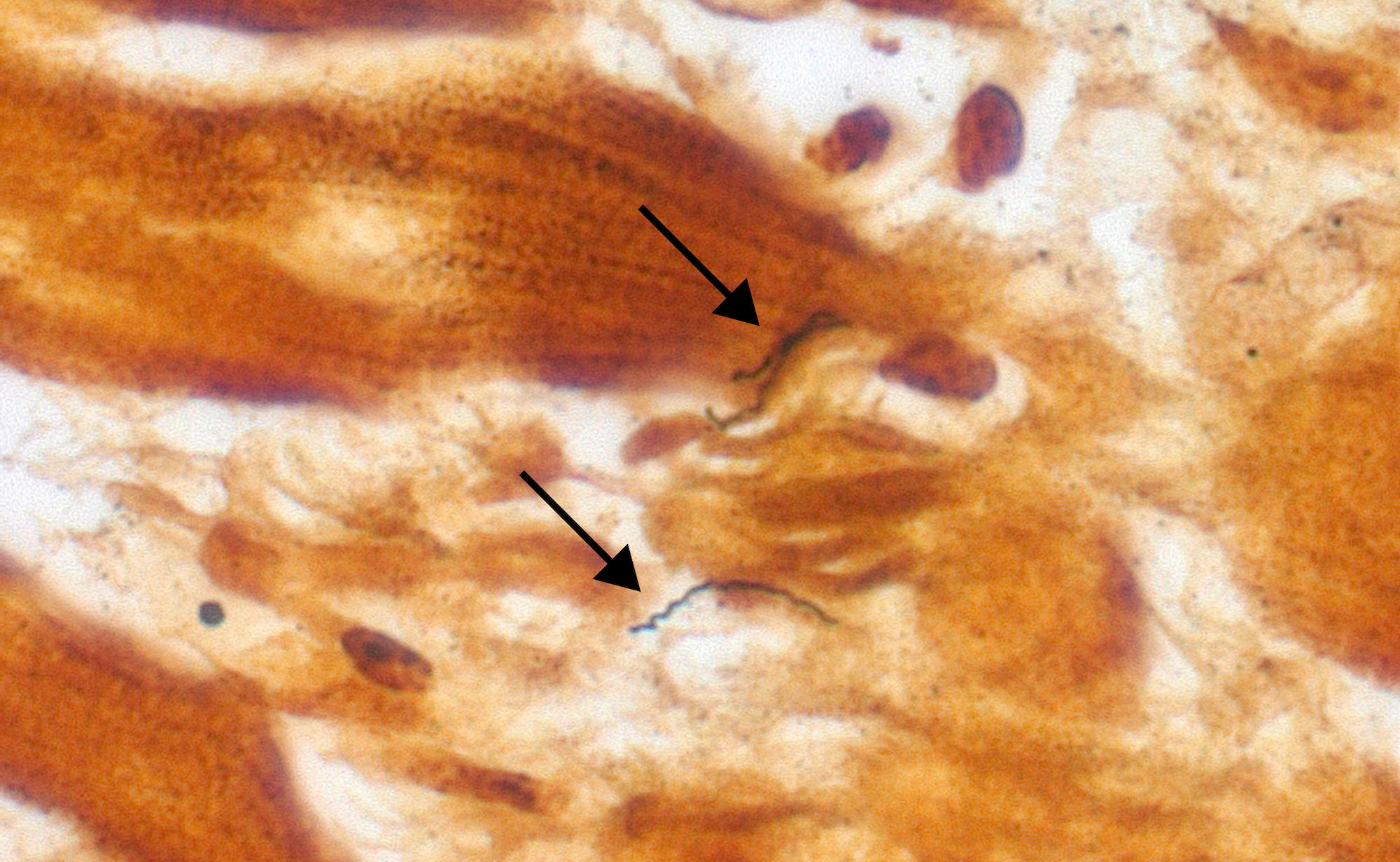
But that’s not the only way tick resistance plays out. Ostfeld says other research shows that some ticks that bite resistant humans are more likely to detach than to die, and a 2020 study showed other effects on ticks like impaired feeding, or inability to molt into their next life stage. Because of the anecdotal evidence and varying nature of tick resistance in people, scientists have limited data on the mechanisms that might help them harness it. And identifying them is a complex task.
Ticks can produce thousands of different proteins in their saliva over the course of their lives. Dr. Thomas Hart, an infectious disease microbiologist at Johns Hopkins University and lead author on the March paper, says that which ones they’re physically releasing into their hosts can change by the hour.
“So a tick that’s been feeding for 30 minutes versus 24 hours versus five days are all gonna be secreting different proteins in saliva,” Hart says. The proteins they produce also change during different stages in their life cycle, from larva to nymph to adult.
This is why Fikrig, Hart, and their team used a tick’s entire genome to produce the proteins a tick makes across its lifespan—over 3,200 of them—and test how a common human antibody reacts to them. They identified almost 200 proteins that could spark an immune response.

Fikrig’s lab has been formulating mRNA vaccines that can encode for the proteins they identified. These vaccines, like the Pfizer and Moderna COVID-19 vaccines, work by exposing cells to mRNA that instructs them to make the proteins carried by their invader. That way, the immune system can learn to recognize and attack them without ever being exposed to the tick. Fikrig says that they used an mRNA vaccine for their experiment because “it’s the easiest, quick way … to ask whether it works or not.”
In 2021, Fikrig’s lab tested an mRNA vaccine that encoded for 19 tick salivary proteins in a small number of guinea pigs and found that it prevented ticks from feeding and reduced Lyme disease transmission. Through their analysis from this year, they identified a new group of 25 proteins in tick cement. They gave three guinea pigs an mRNA vaccine for those cement proteins, and found that ticks detached from them at a significantly higher rate than those vaccinated with a control.
LYMErix, a Lyme disease vaccine that was approved by the FDA in 1998, was a recombinant vaccine that trained the immune system to respond to surface proteins from the Lyme disease bacterium, Borrelia burgdorferi. However, media controversy and reports of adverse side effects led the company behind it to pull the vaccine from the market in 2002.
A new Lyme disease vaccine called VLA15 is in Phase 3 human trials. If approved, it would be a major success in the fight against Lyme. However, some researchers point out that it still wouldn’t protect against the many other tick-borne diseases on the rise like babesiosis, anaplasmosis, Powassan, and more.
“A vaccine against the tick itself makes a lot of sense,” Ostfeld says. “It would be very protective against multiple tick-borne pathogens, and possibly against multiple different species of tick.”
The proteins Hart and Fikrig identified are promising leads on the path to an anti-tick vaccine. The trail is hot, but there’s still much more research needed to formulate a vaccine that could be tested in humans.
“Now is the time to focus,” Hart says. “Really hone in on what are the optimal vaccines … Hopefully we could get the anti-tick vaccine out in the next 10 years or so.”
Emma Lee Gometz was Science Friday’s Digital Producer of Engagement. They wrote SciFri’s “Science Goes To The Movies” series and are a journalist and illustrator based in Queens, NY.