Getting To Know The Placenta
17:32 minutes
Unless you’re a parent, you may not know all the ways the placenta is important to the development of a healthy baby. It provides nutrition, circulates oxygen, and removes waste. But even doctors don’t have an incredibly detailed picture of how the placenta operates during a pregnancy. For instance, how fast can the placenta carry oxygen to the fetus? And how does that impact fetal development?
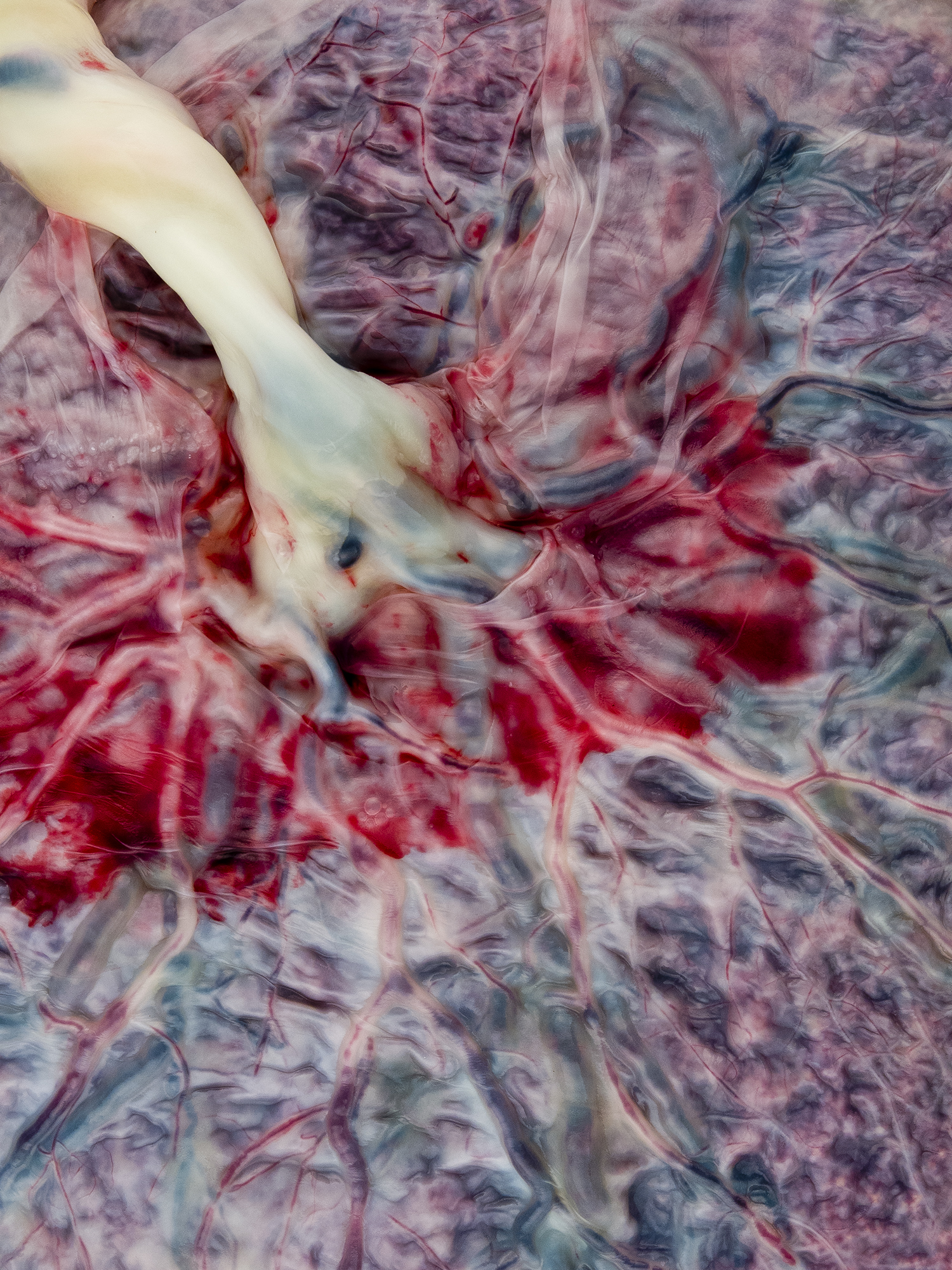
[Witness the hidden beauty of the human placenta.]
In a landmark study of fetal identical twins, an interdisciplinary team of scientists led by Ellen Grant, a professor of radiology and pediatrics at Harvard Medical School, discovered that a shared placenta may deliver oxygen more slowly to one twin than the other. Moreover, less oxygen was correlated with lower liver and brain volumes and lower newborn birth weights. Grant joins Diana Bianchi, the director of the National Institute of Child Health and Human Development, to discuss how studying the placenta is opening doors to a whole new way of monitoring fetal health.
Ellen Grant is a professor of Radiology and Pediatrics at Harvard Medical School in Cambridge, Massachusetts.
Diana Bianchi is Director of the National Institute of Child Health and Human Development, at the National Institutes of Health in Bethesda, Maryland.
IRA FLATOW: I’m Ira Flatow. This is Science Friday. We’re talking now about the placenta, as I said before.
And unless you’re a parent, you may not know all the ways the placenta is important to the development of a healthy baby. It provides nutrition and circulation. And it removes wastes. But even doctors don’t have a very detailed picture of how the placenta is managing all of this during a pregnancy. What we do know comes from studies of the placenta after the baby is born or in animal models.
To measure the function of the human placenta in real time? Well, you can imagine, it’s a much more difficult task, one that a group of Boston based researchers recently undertook. In a landmark study of identical twins in the womb, Dr. Ellen Grant and a team of colleagues discovered that a shared placenta may deliver oxygen more slowly to one twin than the other. Why would the placenta prefer one twin over the other? Well, let’s try to find out.
Dr. Ellen Grant is professor of radiology and pediatrics at Harvard Medical School. Welcome to Science Friday. Dr. Grant, are you there?
ELLEN GRANT: Yes, I am.
IRA FLATOW: Hi.
ELLEN GRANT: Can you hear me?
IRA FLATOW: Yes. Let me–
ELLEN GRANT: Great.
IRA FLATOW: –thank you for taking time to be with us today.
ELLEN GRANT: Oh, no problem.
IRA FLATOW: Let’s talk about your study. Describe what you did to get the results about the oxygen delivery.
ELLEN GRANT: We recruited mothers that had twin pregnancies, so, identical twins. And we asked the mothers to lie in an MRI scanner. And for part of the time, we asked them to breathe 100% oxygen. And we tracked that oxygen from what they were breathing down through the maternal blood, into the placenta, and tracked it across the placenta into the different fetuses.
IRA FLATOW: And so you found that one fetus got more oxygen than the other?
ELLEN GRANT: Yeah. What we did is, we wanted to understand how the placental function might be altering fetal development. So we chose twin fetuses that were very different in size, although identical genetically. And this way, we knew their genetic growth potential was identical, the maternal environment was identical, and their gestational age was identical. So we could look at the placental function by tracking how fast the oxygen traveled across the placenta to the fetus. So we found that in the smaller fetuses, the time that it took the oxygen to reach its maximum value was longer in the smaller twins and the twins that ended up being smaller at birth.
IRA FLATOW: So they were smaller because of the less oxygen they received?
ELLEN GRANT: That’s what we presume, is that the placenta was not functioning as effectively on the side with the smaller twins. And we think that is related to the slower growth in those twins, and probably related to– and further studies are going to explore this more– we think it alters how genes are expressed when you have a different placental in utero environment.
IRA FLATOW: Do you have any idea why one fetus was preferred over the other, received more oxygen?
ELLEN GRANT: It’s not clear. And we don’t understand why there is this discordance in some pregnancies. And up to now, no one’s really been able to monitor the different placenta to see if this might be related to placental function.
But that was one of the exciting things about this study. We could show that the twins that were smaller were related to the placenta with the poorer function. So now we can start to think about, what are some treatments that might be useful, and have a method of monitoring whether treatments are going to be effective.
IRA FLATOW: Mm-hmm. Your study is part of the Human Placenta Project at NIH, which funds research aimed at understanding the role of the placenta in health and disease. So I’d like to bring on the director. Dr. Diana Bianchi is director of the National Institute of Child Health and Human Development at NIH. Welcome to Science Friday.
DIANA BIANCHI: Thank you, Ira. Happy to be here.
IRA FLATOW: And we’re happy to have you. You know, because we never get a chance to talk about the placenta. Many people don’t.
DIANA BIANCHI: Many people don’t talk about it. But everybody was connected to one at some point in their lives. So it’s very important. When you look at your belly button, that’s one end of the placenta. And the other end was connected via the umbilical cord to the actual organ itself.
IRA FLATOW: Now, is the placenta actually considered part of the fetus?
DIANA BIANCHI: So, it’s interesting. Because it has components of both the fetus and the mother. So the majority of it is fetal tissue, genetically. But there’s a back side to it that interconnects directly with the mother’s womb. And that part contains tissue from the mother.
But they’re very closely connected. In fact, to some extent, the placenta invades the mother’s uterine wall. And that’s normal. That should happen.
IRA FLATOW: Now, are there cases where something abnormal goes on when– you know, it does it the wrong way, invading the wall?
DIANA BIANCHI: Yes. Yes, actually. If the placenta doesn’t form normally and the blood vessels connecting to the mother’s blood system don’t form normally, that can result in a condition called preeclampsia, which is truly a life-threatening condition for the mother and results in complications for the baby. And it affects approximately 7% of pregnant women.
IRA FLATOW: Mm-hmm. Let’s talk about this study with Dr. Grant. Did we know anything about how the placenta carries oxygen before this study?
DIANA BIANCHI: Well, we have some indirect measures. So we can measure blood flow by various ultrasound techniques. But the beauty of Dr. Grant’s work is that by giving these mothers extra oxygen, she could track how that oxygen was flowing across the two placentas and really show that the longer it took for the oxygen to flow across the fetal placentas, that that correlated with abnormalities in the particular fetus that had a slower transition of the oxygen.
IRA FLATOW: Mm-hmm. I’m going to give out our number, 844-724-8255, if you’d like to talk about this. And you can also tweet us @scifri, S-C-I-F-R-I. What was the impetus to do this study? Was there something in particular you wanted to study, Dr. Grant?
ELLEN GRANT: Yeah. We really wanted to get at measures that could monitor placental function regionally and throughout the pregnancy. So we wanted to be able to not just look at the placenta after it’s born, but be able to monitor its function during the pregnancy, when it’s actually alive and functioning. And one of the main nutrients that the placenta provides to the fetuses is oxygen. And knowing that we can see oxygen on MRI, we set out to track and quantify how oxygen regionally is passed through the placenta to the fetal blood.
IRA FLATOW: Is this a technique, then, that would be a screening technique for all pregnancies with twins?
ELLEN GRANT: We’re hoping to actually extend it to singletons as well, too. We need a bit more work in terms of creating the equivalent of a growth curve for the placenta across gestation and get a bit better understanding of the differences that can happen due to, say, changes in maternal position, changes in maternal size. So we have a bit of work to do. But that’s the goal, is to have a study that will provide more quantitative numbers of placental function during pregnancy, to help identify those mothers whose placentas are not functioning normally.
IRA FLATOW: Mm-hmm. Dr. Bianchi, do results like this make you think, you know, there’s a lot we still don’t know about?
DIANA BIANCHI: Oh, absolutely. Absolutely. And that’s part of the reason why NICHD, the National Institute of Child Health and Human Development, has dedicated, at the present time, over $54 million in research funding. And currently, we’re funding about 29 projects, about half of which have to do with imaging. All of which are supporting our goal to noninvasively study the placenta in real time, while the woman is still pregnant.
We have a lot of information about the placenta after delivery. But that’s kind of like studying the heart after it’s stopped beating. And so it doesn’t really help us predict what are the complications that are going to occur.
And it doesn’t help us to determine which baby needs to be delivered right now. Because babies can be small for a variety of reasons. You could be genetically predisposed to be small. And that baby should basically stay in the womb. But if a baby is suffering due to lack of oxygen or nutrients, it may be better for both the baby and the mother to be delivered early.
IRA FLATOW: Right.
DIANA BIANCHI: But you’re constantly trying to weigh the risks of an unexpected premature delivery for medical indications versus the risks of staying in the womb when it’s not a good idea.
IRA FLATOW: We’re going to go to the phones. 844-724-8255, if you have questions about placenta and fetal development. And please, keep your suggestions for placenta recipes to yourself. Couldn’t believe it.
Let’s go to a question– let’s go to the phones. Let’s go to Jesse in Rochester. Hi, Jesse. Welcome to Science Friday.
JESSE: Oh, thank you, Ira. So, it sounds like you’ve discovered that the placenta among identical twins would favor one over the other. My twin identical sons had twin-to-twin transfusion syndrome, which sounds like kind of a hyperactive tendency of their placenta to want to feed one and deplete the other. I wonder if you could speak to how your new findings might be related to the twin-to-twin transfusion syndrome.
IRA FLATOW: OK. Could you explain a little more what that is?
ELLEN GRANT: Yeah. Twin-twin transfusion syndrome is when the vessels in the placenta from one twin and the other have abnormal connections. So typically, one twin steals blood from the other twin directly. In our particular study, we excluded twins with those abnormalities. But we’re hoping that moving forward, we can also look at how that transport of nutrients is altered with abnormal connections.
And probably, like anything, the placenta is spectrum. In one spectrum, there is a stealing of blood from one twin to the other. And in another end of the spectrum, there’s one placenta that isn’t functioning as well as it should be. So trying to understand where the boundaries are between normal and abnormal are some of the things we hope to do better as we move forward and can better understand placental function.
And just to clarify, in our study, we specifically chose, on purpose, twins that were different in size. The vast majority of identical twins are very similar in size. And you don’t see this phenomenon.
IRA FLATOW: Mm-hmm. Now, I noticed that you used something called BOLD MRI for this most recent study. How does that work?
ELLEN GRANT: BOLD MRI is Blood-Oxygen-Level Dependent. That’s what BOLD stands for. It means that the signal intensity on an MR image is dependent on the oxygen concentration. It’s actually the sequence that’s used for functional imaging as well, too, except for the oxygen changes are due to neuronal demand. Here, we gave the mothers oxygen and exposed them to oxygen, and tracked that oxygen through the blood, using an image that changes in brightness when the oxygen reaches the vessels.
IRA FLATOW: All right. Let’s go to the phones, to Boulder, Colorado, with Erin. Hi. Welcome to Science Friday.
ERIN: Hi. How are you doing?
IRA FLATOW: Hi there.
ERIN: Hi. I have a question. I had two placentas. I was pregnant with my second child. I had two placentas. And there was only one baby. And the doctors couldn’t explain why.
When the baby was actually born, by c-section– because the other placenta was covering my cervix, so I had to have a c-section– they discovered that I had a velamentous umbilical cord, which means that it wasn’t fully attached. So I was wondering if you had any ideas why there were two placentas. Because they didn’t have any idea– or, if they did have an idea, they didn’t want to tell me. But–
IRA FLATOW: OK. Thanks for calling.
ELLEN GRANT: Yeah, it’s–
DIANA BIANCHI: Well–
ELLEN GRANT: –possible that– oh, go ahead, Diana.
DIANA BIANCHI: No, I was going to say– so my background is, I’m a geneticist and a neonatologist. And I was going to say that one possibility is that there was actually a twin pregnancy, but not necessarily identical twins. So one of the twins could have had a specific reason, like a genetic abnormality, for dying in the womb. But when there’s another placenta there, it can actually keep the second placenta alive, even though long ago, probably early in the pregnancy, the second fetus might have died naturally.
IRA FLATOW: Mm-hmm. Our number, 844-724-8255. You’re listening to Science Friday from PRI, Public Radio International. We’re talking about everything placenta.
And suddenly the boards have lit up. A lot of people interested in the placenta. Let’s see if we have– oh, we have some tweets coming in.
Can you ask your guests about– Johan wants to know about single umbilical artery. Usually there are two. What’s the biology of having just one? Anybody know that one?
DIANA BIANCHI: Well, it is what we call a minor malformation. It’s not infrequent. You have to have at least one. But I’m aware of people having anywhere between 1 and 4, even though 2 is the more common number. But that in and of itself shouldn’t have any long-term consequences. Unless it was associated with other malformations.
IRA FLATOW: Here’s a question. Should we recommend now that pregnant women take a little extra oxygen if they’re carrying twins?
ELLEN GRANT: I think we don’t really understand the answer to that yet. There are some disorders where they’re considering that, like women who have fetuses with congenital heart disease, for example. But we don’t know what the long-term effects are of oxygen exposure.
And it may shift the metabolism of the placenta. So it’s not clear that oxygen would improve long-term function versus just change the metabolic state of the placenta at the detriment of the fetus. So we need to study that more to really make recommendations.
IRA FLATOW: Here’s a call from San Francisco, from Alyssa in San Francisco. Welcome to Science Friday. Hi there. Hi. Go ahead.
Well, I think it’s a cell phone problem. Sounds like it. She was going to ask, could this study be used to predict small stature in twins?
ELLEN GRANT: In the small group we studied, this preliminary study, we predicted the birth size. But that’s not predictive of stature long-term. So we haven’t been able, at this point in time, to come up with– these measures don’t look like they’re going to be able to predict height.
IRA FLATOW: Dr. Bianchi, what other research is coming out of the Human Placenta Project?
DIANA BIANCHI: Well, again, so the focus is noninvasive and in real time. So we’re focusing on different aspects of imaging. We’re also focusing on things that we can determine from blood samples in pregnant women.
So we’re looking at RNA, one of the nucleic acids. We’re looking at lipids. We’re looking at the microbiome. And we’re trying to determine whether, if you take a blood sample from a pregnant woman, that we would get additional information about the biology or the health of the placenta.
IRA FLATOW: And how long will your study go on, the project go on for?
DIANA BIANCHI: Yeah. So the project started in 2015. And the first group of projects started with development of novel technologies, such as Dr. Grant’s project. And most of the grants are now in their first cycle. So they’re somewhere between three and five years. And then we will re-evaluate what we’ve learned.
IRA FLATOW: Mm-hmm. I want to thank you all for taking time to be with us today. It’s an interesting new topic we have never discussed.
Dr. Ellen Grant, professor of radiology and pediatrics at Harvard Med School. Dr. Diana Bianchi, director of the National Institute of Child Health and Human Development at NIH. Thank you for being with us. Have a good weekend.
ELLEN GRANT: Thank you, Ira.
DIANA BIANCHI: You, too.
IRA FLATOW: You’re welcome.
ELLEN GRANT: You, too.
IRA FLATOW: When we come back– we’re going to take a break first, and then talk about new additions to the atlas of exoplanets. Pack your bags. Because there are a lot more new exoplanets that have come onto our radar.
They were all discovered– we’ll talk about the new list of 4,000 potential distant worlds. 4,000. 10 that could be rocky planets. We’ll talk about it after the break. Stay with us.
Copyright © 2017 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of ScienceFriday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Katie Feather is a former SciFri producer and the proud mother of two cats, Charleigh and Sadie.