How Does The Appendix Play A Role In Parkinson’s Disease?
10:52 minutes
You’ve probably heard that you don’t necessarily need your appendix, especially if you’ve had it removed. But the appendix does have a function and scientists are learning more about how it affects our health. The organ plays a role in regulating the immune system, microbiome, and even Parkinson’s disease.
A misfolding in the protein called alpha-synuclein has been linked to Parkinson’s disease, and researchers found abnormal clumps of this protein in the appendix. This week, a team of scientists found more evidence for the link. Reporting in the journal Science Translational Medicine, the researchers found that, for Parkinson’s patients, there was a 3.6 year delay in onset of the disease for those who had an appendectomy.
[These bats are very precise flyers.]
Neuroscientist Viviane Labrie, who is an author on the study, talks about how the proteins could move from the appendix to the brain, and what this means for diagnosis and treatment of the disease.
Read the original study in Science Translational Medicine.
Viviane Labrie is an assistant professor at the Center for Neurodegenerative Science at the Van Andel Research Institute.
IRA FLATOW: This is Science Friday. I’m Ira Flatow. You’ve probably heard that you don’t need your appendix. So who hasn’t heard that? You can have your appendix out. It’s just a vestigial organ. Doesn’t do much for us anyhow, especially if you’ve had it taken out.
Well, that may not be entirely true. There is evidence that the appendix plays a role in regulating our immune system, our microbiome, and even Parkinson’s disease. New research shows that a key protein linked to the development of Parkinson’s disease is found in the appendix. Scientists found that in Parkinson’s patients who’d had an appendectomy, onset of the disease, was delayed by nearly four years.
These findings were published in the journal Science Translational Medicine. So how does the appendix connect to a movement disorder like Parkinson’s, and should we be rethinking our appendix? Viviane Labrie is an author on that study. She’s also an assistant professor of neuroscience at Van Andel Research Institute in Grand Rapids, Michigan. Welcome to Science Friday.
VIVIANE LABRIE: Thank you.
IRA FLATOW: We’ve often heard that we didn’t really need our appendix.
VIVIANE LABRIE: Yeah. Normally when you think of the appendix you think of this useless organ. It’s attached to the large intestine and an appendectomy is a very common surgical practice. But as it turns out, the appendix does have a function in our bodies. It plays a role in the immune system and it regulates the microbiome.
So we know that inflammation has been linked to Parkinson’s disease and there’s changes in the microbiome in Parkinson’s patients. And the microbiome, the gut bacteria of your intestine can regulate brain health. So this small tissue is actually an immune tissue, which samples and monitors pathogens and will raise immune responses, and as a storage house for the gut bacteria in your intestine.
IRA FLATOW: And so does the gut bacteria travel then up to your brain from the appendix?
VIVIANE LABRIE: No. The gut bacteria will communicate with the immune system. It can also modulate the firing of nerve cells in the GI tract.
IRA FLATOW: Your study found that in people who had their appendix removed, their risk was 20% lower compared to those who still had their appendix. What do you think is happening there?
VIVIANE LABRIE: So in our study we looked at big medical history data sets and we found when we looked at 1.6 million people that there was a lowered risk for Parkinson’s disease. In fact, the risk was lowered after an appendectomy by nearly 20%. But the appendectomy had to have happened in early life. So an appendectomy occurring 20 or more years before the onset of Parkinson’s symptoms.
So most people have an appendectomy in their 20s, and then if Parkinson’s were to develop, that would be in their early 60s. And so what we think is happening is that the appendix could be involved in the early events or even in the triggering of changes that could lead to Parkinson’s disease.
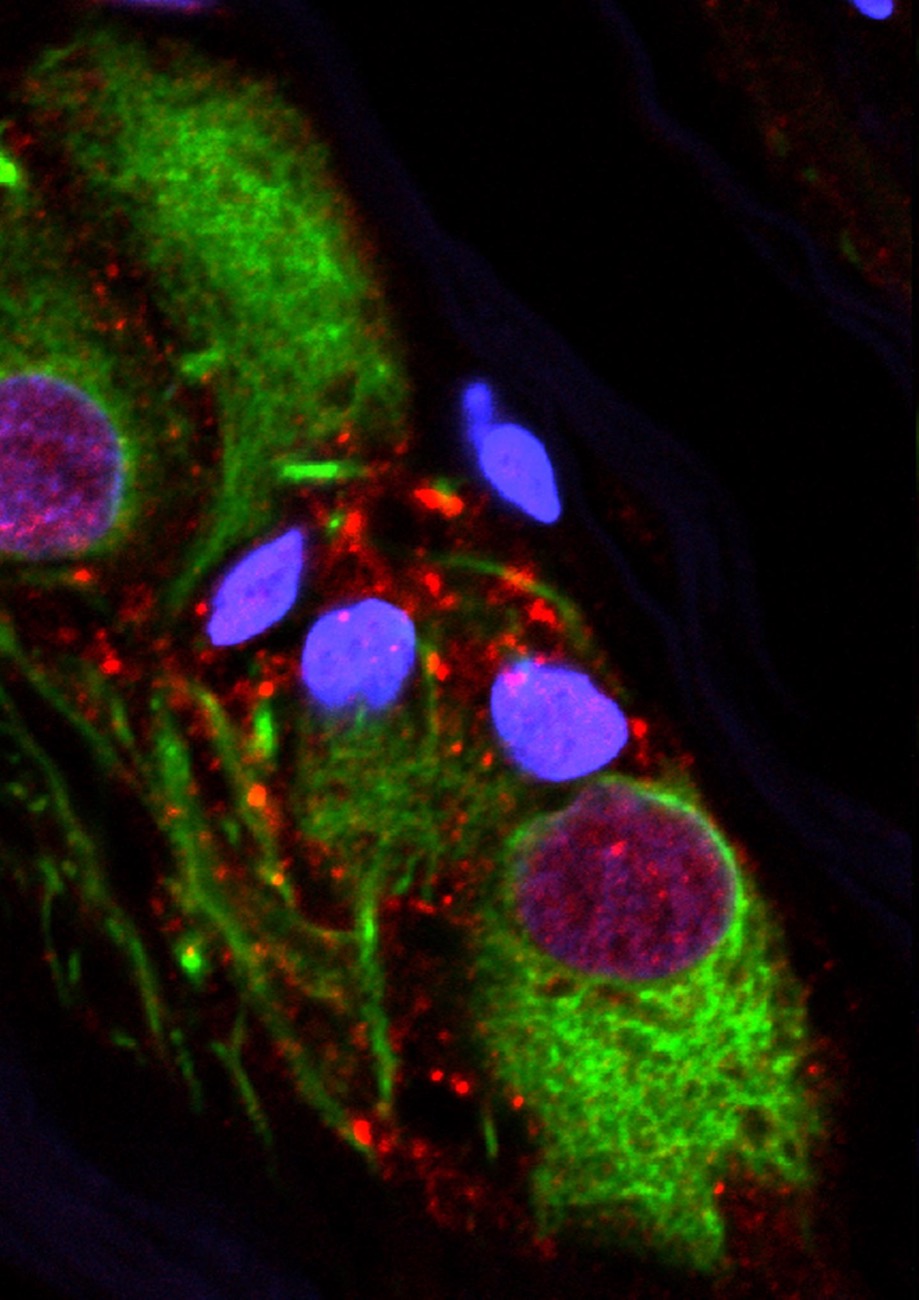
And that’s because when we looked inside the appendices of healthy individuals, as well as eventually we studied the appendix of Parkinson’s patients, we found an abundance of this clumped protein called alpha-synuclein. Now alpha-synuclein is a protein that makes up the hallmark pathology of Parkinson’s disease. It Lewy bodies they’re called. And these are found in the Parkinson’s brain.
And what we saw in the appendix of even in healthy people that the clumped protein alpha-synuclein was present in the nerve cells and very much resembled the protein that you would find in Lewy bodies in the Parkinson’s brain. So what we think might be happening is that if the clumped protein were to accumulate in excess and potentially have escape and travel up nerves that connect the GI tract to the brain, this could have disastrous consequences that could lead to eventually Parkinson’s disease.
IRA FLATOW: It’s fascinating. Are we recommending people then have appendectomies or not have them?
VIVIANE LABRIE: One thing we’re definitely not recommending is for people to go out and have preventative appendectomies. We’re also not suggesting that just because you have an appendix you’re going to get Parkinson’s disease. But what we are saying is that the human appendix, even under normal circumstances, contains an abundance of this clump protein we associate with Parkinson’s disease.
So what distinguishes a Parkinson’s patients from a healthy individuals is not the presence or absence of this clump protein as we once thought, but perhaps a difference in the ability to manage this pathology. So if in some people it were to accumulate in excess and travel up nerves that connect the GI tract to the brain, this could cause Parkinson’s disease.
IRA FLATOW: If there is a definite connection or a strong connection, why is the percentages not different, much higher percentages instead of a 20% or 40%, something like that? Why not 70%, 80%?
VIVIANE LABRIE: So Parkinson’s disease is really an umbrella term for a disorder that involves multiple trigger sites. So for some people, it may start in the GI tract. And so there is evidence that the pathology associated with Parkinson’s disease is seen in patients even years before the onset of motor symptoms.
We also know that this pathology, this clump protein called alpha-synuclein is a protein that doesn’t like to stay put. It’s able to travel between neurons and neurons, nerve cells to nerve cells. And there’s our nerves that connect the GI tract to the brain. It’s called the vagus nerve. It’s not the longest nerve in the body, but it’s certainly a very long one. And we know that this protein can travel up this nerve and enter the brain and seed and spread from there.
For other individuals, the disease might start in the brain or elsewhere in the body. So Parkinson’s disease encompasses multiple trigger sites. What’s surprising is that some of those trigger sites might be outside of the brain.
IRA FLATOW: That is surprising, isn’t it? Yeah. I’m trying to so to speak digest it. We talk a lot about the microbiome on Science Friday. So we’re sort of connecting it in with the microbiome here, are we not?
VIVIANE LABRIE: Right. So the microbiome in Parkinson’s patients is known to be different. And those changes are still being described, but differences in the microbiome can affect brain health. So it can affect the singling of nerves. It’s also known to change mood like anxiety and depressive symptoms.
So there’s other symptoms in Parkinson’s disease, such as the nonmotor symptoms, which do involve things like depression. So you could have the microbiome regulating the neurodegenerative aspects, but also the cognitive or the anxiety symptoms as well on the depressive symptoms. So the microbiome is a complex thing.
It’s made up of different bacteria. And if the bacteria ecology were to shift to say a proinflammatory microbiome and if that proinflammatory microbiome or to be housed in say the appendix, which helps regulate the gut bacteria in the rest of the GI tract, that could have disastrous consequences. The other thing that I want to mention is that the appendix is really important in the immune system.
And so inflammation has also been tied in to Parkinson’s disease, inflammation specifically in the GI tract and in the brain. And they know that if there is a lowered risk, that’s associated with Parkinson’s disease in people that take a compound that reduces GI tract inflammation.
We also know that different illnesses like Crohn’s disease have a greater risk. This is a disease that involves GI tract inflammation. These individuals have a greater risk for developing Parkinson’s disease. So there seems to be connections related to the immune system, the microbiome, and this clump protein called alpha-synuclein and its ability to seed and spread.
IRA FLATOW: So what would you like to know now that you know this? Where do you go from here?
VIVIANE LABRIE: Well, we were really surprised to find the pathology associated with Parkinson’s disease, this clump protein alpha-synuclein in the appendixes of healthy individuals. And we looked at young individuals under the age of 20, older individuals inflamed or noninflamed. It was in everybody.
And so that made us realize that Parkinson’s disease wasn’t defined by this pathology. It’s very normal to be present in the appendixes of people. But if that pathology were to travel to the brain and enter the brain, that has neurotoxic effects.
So location is everything. Clump protein alpha-synuclein in the appendix very normal; clump protein of alpha-synuclein in the brain, neurotoxic. And so what we think is going on is that there’s possibly a difference in ability to manage this pathology between healthy individuals and people who will go on to develop Parkinson’s disease.
And what we want to get down to is those molecular mechanisms that will distinguish a healthy individual from a Parkinson’s person. And that will help us develop markers and perhaps improve the targets and develop new treatments for this illness. That would involve treatments that would be very exciting because they would target the GI tract instead of the traditional treatments, which are focused on things that are happening in the brain. So it opens up a whole new avenue of therapies for Parkinson’s disease.
IRA FLATOW: Very interesting. We had a tweet from Lisa, who said, what about the effects of diet? Could diet then because we’re talking about the GI area and we’re talking about the appendix also play a role here?
VIVIANE LABRIE: Well, I think that diet and inflammation do tie into each other. So good eating, good sleeping, exercise, all of these things are beneficial to the immune system. And so anything that can kind of help dampen down inflammation in the area that the GI tract– now remember, the GI tract has an abundance of nerve cells.
It’s sometimes called the second brain because it has so many neurons– it’s more than even the spinal cord. Not as much as the brain but more than the spinal cord. And so if we were to turn down an inflammation, which has a close communication with nerve cells in the GI tract, that could only be a benefit. And so things like diet and exercise and good sleep are ways of doing that.
IRA FLATOW: Dr. Labrie, thank you for taking the time to be with us today. Fascinating.
VIVIANE LABRIE: Thank you. My pleasure.
IRA FLATOW: Viviane Labrie is an assistant professor of neuroscience at the Van Andel Research Institute in Grand Rapids, Michigan.
Copyright © 2018 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Alexa Lim was a senior producer for Science Friday. Her favorite stories involve space, sound, and strange animal discoveries.