Using Stem Cells For Cornea Repair Is Worth A Look
12:16 minutes

Each year in the US, over 40,000 people receive transplants of the cornea—the clear front part of the eye that light goes through first. Still more patients with damaged corneas might receive artificial corneas to help restore clear vision. But if an eye has been damaged by a chemical burn or another severe eye injury, neither of those treatments may be possible.
Now an early, Phase 1 clinical trial is reporting positive results using a stem cell technique called CALEC. It grows cells from a patient’s healthy eye, and then grafts them back into the damaged eye, either to support corneal tissue regrowth or as a foundation for a traditional transplant.
Dr. Ula Jurkunas, associate director of the Cornea Service at Mass Eye and Ear, and Dr. Jerome Ritz, the executive director of the Connell and O’Reilly Families Cell Manipulation Core Facility at Dana-Farber Cancer Institute, join Ira to talk about how the process works, and the challenges of manufacturing stem cell tissues in the lab for use in the human body.
Dr. Ula Jurkunas is associate director of the Cornea Service at Mass Eye and Ear in Boston, Massachusetts.
Dr. Jerome Ritz is the executive director of the Connell and O’Reilly Families Cell Manipulation Core Facility at the Dana-Farber Cancer Institute in Boston, Massachusetts.
IRA FLATOW: This is Science Friday. I’m Ira Flatow.
KATHLEEN DAVIS: And I’m Kathleen Davis. A bit later in the hour, we’ll look ahead to the Women’s World Cup finals with a new book about women athletes and look at the world in a grain of sand.
IRA FLATOW: But first, each year in the United States, some-40,000 people receive transplants of the cornea. That’s the clear front part of the eye that light goes through first. Other people receive artificial corneas to help restore clear vision. But if an eye has been damaged by, let’s say, a chemical burn or another severe eye injury, those treatments may not be options.
But now, an early Phase 1 clinical trial is reporting positive results using a stem cell technique to grow cells from a patient’s healthy eye that can then be placed back into the damaged one. Joining me to talk about this are two guests involved in the study. Their work is reported in the journal Science Advances.
Dr. Ula Jurkunas is associate director of the cornea service at Mass Eye and Ear in Boston. Dr. Jerome Ritz is the executive director of the Connell and O’Reilly Family Cell Manipulation Core facility at Dana-Farber Cancer Institute in Boston also. Welcome to Science Friday.
JEROME RITZ: Thank you.
ULA JURKUNAS: Thank you.
IRA FLATOW: Nice to have both of you. OK, let’s start with eye 101. Dr. Jurkunas, let’s talk about what the cornea is first, OK?
ULA JURKUNAS: So the cornea is the clear dome that is the front layer of the eye. And the reason it is clear is because there are stem cells that reside in the periphery of the cornea. And these corneal stem cells prevent the white part of the eye, or conjunctiva, from growing onto the cornea and maintain the corneal clarity.
IRA FLATOW: Is this just a specialized form of skin? What is it made out of?
ULA JURKUNAS: So they are actually adult-like stem cells. Believe it or not, our bodies have stem cells even though we are adults, and they are the source of corneal epithelium or surface of a cornea. They are kind of like skin cells, but they are transparent unlike skin. There are various conditions that damage those cells. And when that happens, the cornea loses its transparency.
IRA FLATOW: But skin cells, some damage, when we damage our skin, the skin grows back. And with a certain amount of damage to the cornea, not a lot, that will grow back, too, correct?
ULA JURKUNAS: That’s right. Sometimes when we get a scratch on the cornea, that heals right away. However, if we really deplete those stem cells from severe injuries or infections, then those cells do not grow back.
IRA FLATOW: Mm. Now, I mentioned cornea transplants, and they often are successful for many patients. Why can some people not get them?
ULA JURKUNAS: So if you don’t have stem cells, you can replace the central cornea with a new cornea, but it will never take as these stem cells will not be there to regenerate the front layer of the transplant. And again, the conjunctiva will overgrow the clear part of the cornea.
IRA FLATOW: Hmm. We’ve heard so much about transplants. Could you walk me through the basics of how a transplant works?
ULA JURKUNAS: So the transplantation system is really well developed in our country. We receive a lot of donor corneas that are from grateful families that donate their loved ones’ corneas, and these corneas are transplanted onto our patients. However, these patients usually have to have very healthy peripheral stem cells, and then the transplant works well.
IRA FLATOW: Now, Dr. Ritz, your job is to grow these special stem cells in your lab. It’s sort of a manufacturing process, if you will?
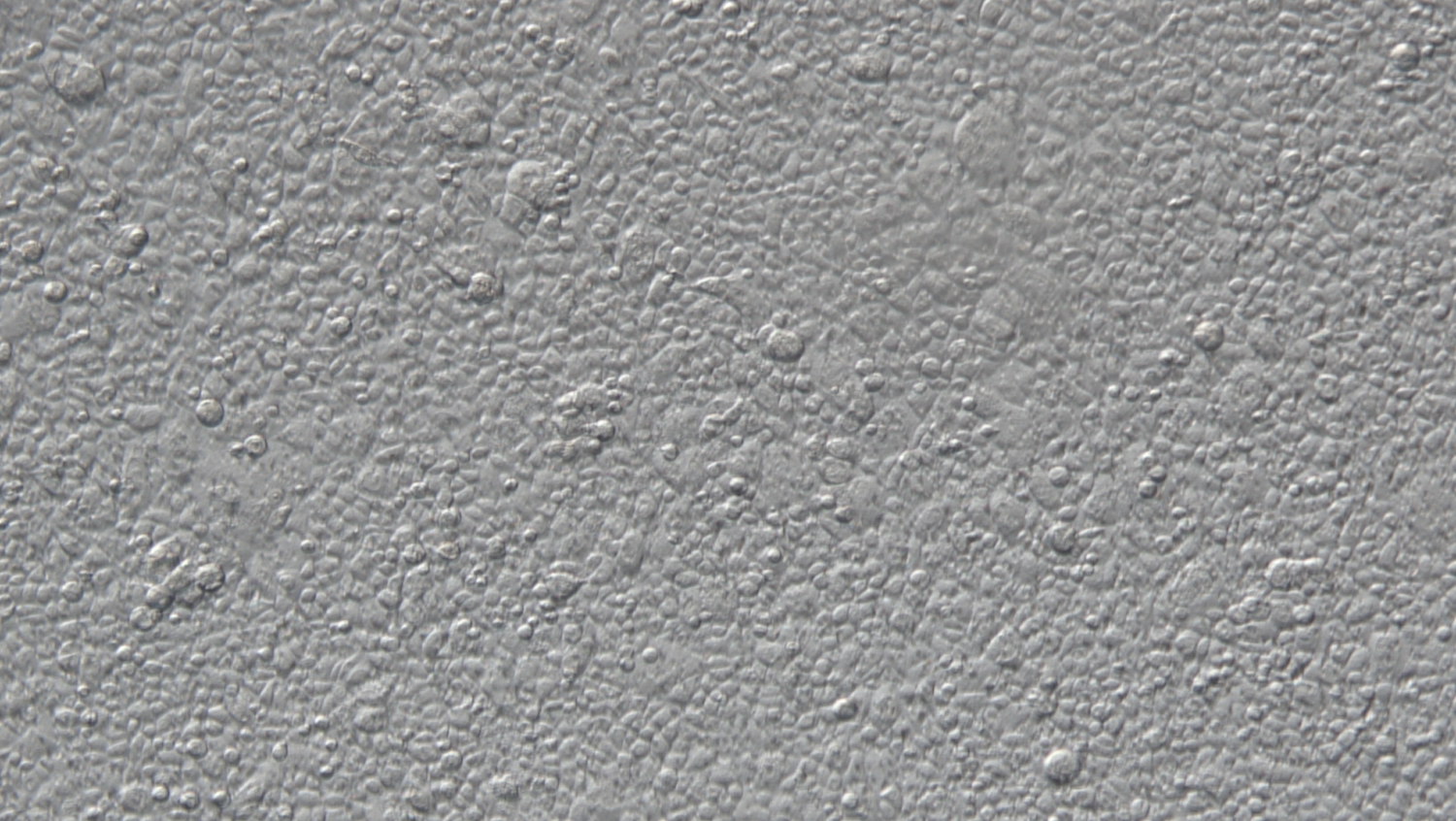
JEROME RITZ: That’s correct. What we do in this process is we get a small biopsy that Ula takes in the operating room from the good eye. There’s a small biopsy that contains the stem cells, and they come into our laboratory. And then we use those cells to create what we call this culture, the CALEC, this cultured autologous limbal stem cell graft.
IRA FLATOW: To get the cells to grow properly, you need a kind of template, a membrane. What does that look like?
JEROME RITZ: So the process that we developed is a two-stage process. One is we take the biopsy, and we isolate little pieces of it. And these limbal stem cells grow out on plastic, just in a plastic dish. And then once we get enough cells– and that takes about a week or a week and a half– then those cells are then transferred onto an amniotic membrane.
This is a membrane that is used commonly by ophthalmologists in their surgical procedures. We use it in the laboratory to use as a substrate. And then when the cells grow over it and become confluent, then we’re finished. And then we take that, package it up, and send it back to the Mass Eye and Ear for Ula and her team, who will use this and sew it back into the patient’s cornea.
IRA FLATOW: So you’re not actually growing a whole new cornea, just the cells needed to support the cornea?
JEROME RITZ: Correct, yeah.
IRA FLATOW: So give me an idea how big it is. Is it a square inch, a square centimeter?
ULA JURKUNAS: Yeah, so actually, when we transplant, the cells come in a little container from Jerry’s lab. And then we take them out from these wells of a culture plate. And I usually use a 17-millimeter trephine, so it’s almost 2-centimeter size that is of a membrane. And then we suture it to the eye with very, very thin sutures. They are actually thinner than hair. They call it 10-0 nylon suture.
JEROME RITZ: Yeah, so what I would add is that the other part of the process is we put the cells on this membrane, and that membrane is used to place those cells in the right position, as Ula mentioned. But then eventually the amniotic membrane that’s used will dissolve and will actually get resorbed over time, leaving only the stem cells.
IRA FLATOW: So just to repeat, once these cells are grown by Dr. Ritz, you put them into the damaged eye?
ULA JURKUNAS: Yes. Once the cells are grown and come from Dr. Ritz’s laboratory, they are transplanted or placed on the donor eye after careful removal of a scar tissue because a lot of times patients have a lot of scar formation from their injury.
IRA FLATOW: And how well does that work?
ULA JURKUNAS: Well, it actually immediately is quite better. It takes some time for the cells to really adhere and for the cornea to heal. Our study shows 12-month data, so it’s actually very encouraging. And the next step is our longer follow-up data of 18 months. That is in the preparation right now.
IRA FLATOW: So basically, what you’ve proven is a proof of concept that this can work. Would that be correct?
ULA JURKUNAS: I think that we showed that it is feasible to employ body’s own stem cells and to grow them and to place them back in a patient, and it’s also safe. The efficacy data is the next step for us to show.
IRA FLATOW: And so in your study, how successful were you in actually helping people with their new corneas?
ULA JURKUNAS: I think a lot of times in science, we want to leave the word success until we have a little bit stronger evidence and follow-up and kind of a data analysis. However, case-by-case reports of those four patients have shown an improvement in quite a few parameters and definitely decrease in their pain and symptoms.
IRA FLATOW: Mm-hmm. And does the cornea heal over these cells itself, or do you need to use it as a substrate for a regular corneal transplant?
ULA JURKUNAS: This is a great question. So out of four patients, two patients actually have improved, and they did not need further transplantation. However, two people did require a standard transplant in what we call in the bed of the stem cells. So the stem cells kind of engrafted or started growing and living in that new cornea, so to speak, and then we placed a corneal transplant on top of it. And the survival of those transplants indicates that the stem cells are indeed there and they are functioning.
IRA FLATOW: Very cool. OK, so give me the timeline for future studies and making this more available because when people hear you on this program talk about this kind of research, they want to know how to get it for themselves or other people.
ULA JURKUNAS: Well, it’s a little bit hard to [LAUGHS] answer because right now we are analyzing the data of our larger study, so Phase 2A. And then the next step will be to form even larger study, maybe multicenters trial. This was 1 center, one manufacturing facility. Hopefully, the next study will be to do many more patients and with several different manufacturing facilities and different surgeons performing the procedures.
IRA FLATOW: Interesting. Dr. Ritz, is there something you have learned from this process that you’ve developed that could let you grow other kinds of eye cells, maybe a new retina, let’s say?
JEROME RITZ: Yes, I think these cells are very different than retinal cells. So I’m not sure it would be applicable to that, but there are other stem cell projects that we’re working on in our facility. It is now possible to generate what are called induced pluripotent stem cells from normal cells in the body.
And once you’ve generated these IPS cells, then those cells can be differentiated into a variety of different cell types. And there are a lot of studies going on in our lab and around the country using these IPS cells to create more differentiated cells. There are studies that are being done using these cells to generate cells that secrete insulin, for example, for patients with diabetes.
There are studies to use these cells to create dopaminergic neurons for patients with Parkinson’s. So I think that we’re really just in the very beginning of the field of using stem cells to create tissues, and I think this project using limbal stem cells to create this cornea is, I think, one of the areas that I think is going to be very successful.
IRA FLATOW: Dr. Jurkunas, do these eye stem cells need to be matched to the donor? I mean, could we get to the point where you could use stem cells taken from someone else’s eye?
ULA JURKUNAS: I think that is the future of this cell therapy. This first proof-of-concept study showed that it is possible to actually expand stem cells and to regenerate corneas, but definitely the next step is to use allogeneic, meaning another person’s, stem cells to help the other person because a lot of corneal blindness and stem cell deficiency is bilateral, meaning in both eyes, and we may not have a source of both stem cells in the same individual.
I think that the future is really bright. And with some manipulation maybe even to altering that immunogenicity that maybe Jerry can work on, we could potentially provide stem cells for others from one donor to another.
IRA FLATOW: Well, this has all been very exciting. We have run out of time. I want to thank both of you for joining us today, and good luck with your research.
JEROME RITZ: Thank you very much.
ULA JURKUNAS: Ira, thank you so much.
JEROME RITZ: You’re welcome. Dr. Ula Jurkunas is associate director of the cornea service at Mass Eye and Ear in Boston and Dr. Jerome Ritz executive director of the Connell and O’Reilly Family Cell Manipulation Core facility. That’s at the famous Dana-Farber Cancer Institute, also in Boston.
Copyright © 2023 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
As Science Friday’s director and senior producer, Charles Bergquist channels the chaos of a live production studio into something sounding like a radio program. Favorite topics include planetary sciences, chemistry, materials, and shiny things with blinking lights.