Tracking Pain In Your Brain
9:46 minutes
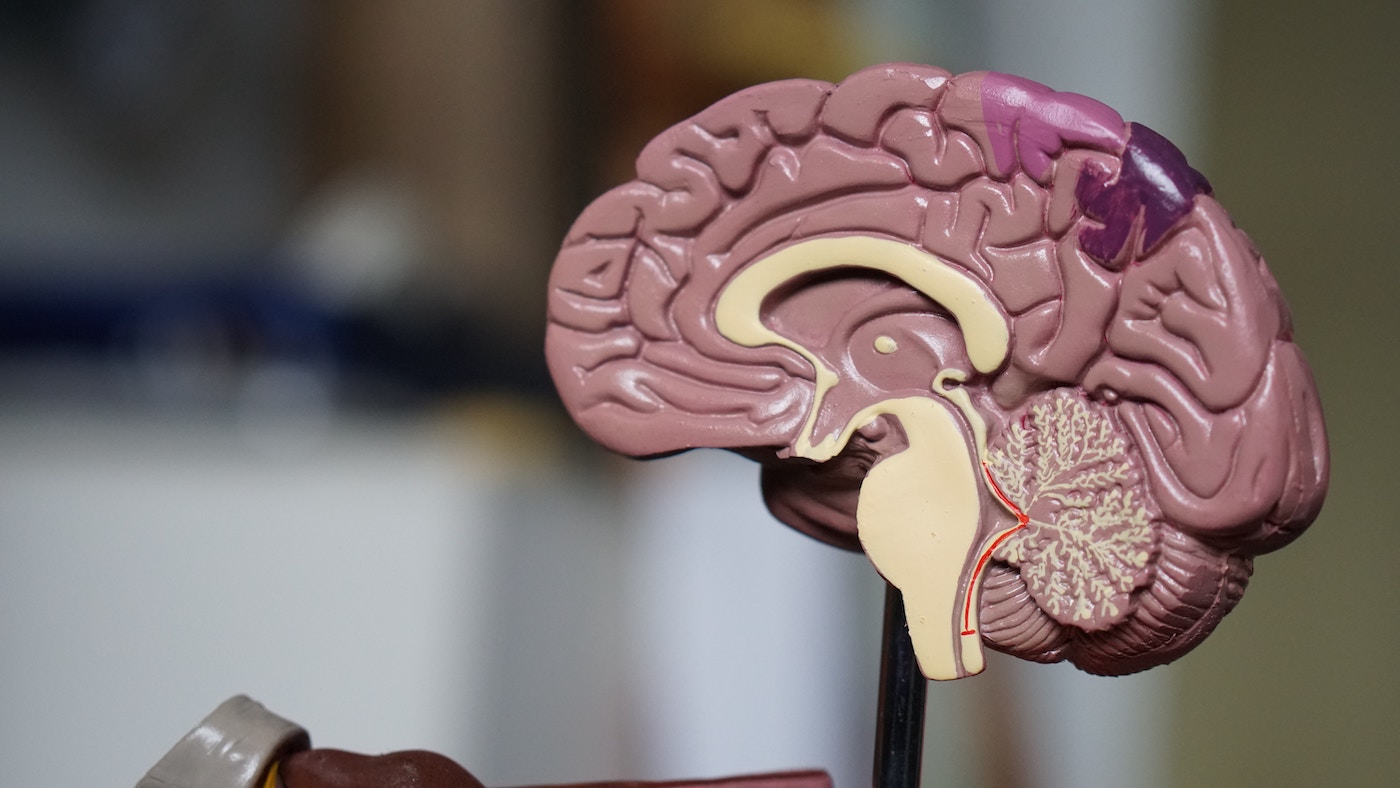
When you stub your toe, that pain is registered by the peripheral nervous system. It shoots off signals that travel up your spinal cord and to your brain, where the signals tell you, “Hey, your toe hurts. Take care of it.” But chronic pain—defined as lasting three months or more—is processed differently, and your nerves are constantly firing pain signals to your brain.
Chronic pain is complex, and a lot of its basics are still unknown. But a new study from this week discovered another piece of the pain puzzle: brain signals that are associated with chronic pain and the region they are processed in. Researchers hope that this is the first step in developing a brain stimulation therapy that can intercept those chronic pain signals and bring relief to patients.
Guest host and SciFri director Charles Bergquist talks with lead author Dr. Prasad Shirvalkar, neurologist and associate professor at the University of California San Francisco, about this new paper.
Invest in quality science journalism by making a donation to Science Friday.
Dr. Prasad Shirvalkar is a neurologist and an associate professor at the University of California San Francisco in San Francisco, California.
FLORA LICHTMAN: This is Science Friday. I’m Flora Lichtman.
CHARLES BERGQUIST: And I’m Charles Bergquist. When you go to the emergency room, one of the first questions someone usually asks is, rate your pain on a scale from 0 to 10. That helps doctors decide how to treat you. But how do I know that my 8, for example, is the same as your 8?
Pain is subjective. And it can vary. Maybe some days are less painful than others. A team of doctors set out to actually put a number on pain, to see if there’s an objective way in the brain to measure and diagnose it, especially chronic pain, which by definition, lasts three or more months and can be debilitating.
Here to talk about this study is lead author Dr. Prasad Shirvalkar, neurologist and associate professor at the University of California San Francisco. Welcome to Science Friday.
PRASAD SHIRVALKAR: Thank you, Charles. It’s great to be here.
CHARLES BERGQUIST: It’s so great to have you. First of all, what’s the difference between my brain registering pain when I do something like whack my elbow or sprain my wrist versus the chronic pain that we’re talking about?
PRASAD SHIRVALKAR: Yeah, so chronic pain I think of as truly a separate disease than an acute or short lasting pain like whacking your elbow or stubbing your toe. When you have immediate acute pain, what happens is, your peripheral nerve endings signal electrical signals to your spinal cord, which ultimately reach your brain. And they create this perception of alert or threat.
It’s inherently unpleasant, right? But what’s a big mystery– and the study that we published helps, I think, provide the first clues to unravel this mystery a little bit is, over the three months that chronic pain develops from acute pain, we don’t really understand what changes take place in the spinal cord or the brain in the real world.
And so something happens where there’s rewiring between brain regions, between circuits in the spinal cord, and even in the peripheral nerves where chronic pain reflects a reorganization where acute pain signals, we think of as primarily living in the peripheral nerves and spinal cord, undergoes some kind of transition where chronic pain, these signals are more represented in the brain in unique ways.
Where in the brain that are represented and how they’re distributed across the brain, it’s still puzzling. But it’s clear that chronic pain involves a much greater emotional component– we call it the affective component– than the acute pain or even some kind of transient pain.
Chronic pain also is associated with much more significant suffering. It bleeds into people’s relationships and their moods from a day-to-day basis and often makes it really hard to focus attention, which is actually an unfortunate paradox because one of the coping mechanisms people use for chronic pain is to actually try to shift their attention away from their pain and onto other things to try to distract themselves.
And chronic pain is actually associated with a host of brain changes but also changes in someone’s social life, in their personal psychology. And so it really infuses into, I think, every aspect of an individual’s waking life as opposed to acute pain, which we hope, with time, will heal, right?
CHARLES BERGQUIST: I mean, as you say, it seems hard to quantify. How do I know that my sense of the color blue is the same as your sense of the color blue? But you’re trying to put a number on this. Tell me how you did that.
PRASAD SHIRVALKAR: Yes, so it’s absolutely hard to compare between individuals. And you’re right, your blue is probably different than my blue. And I don’t even know if that’s knowable.
Nonetheless, the study we did is part of a larger clinical trial aimed at developing new, personalized brain stimulation therapy for chronic pain. So as part of this trial, we surgically implanted electrodes to target two brain regions that we think are involved in pain. That’s the anterior cingulate cortex and the orbitofrontal cortex.
These electrodes were implanted surgically in four patients who were suffering from chronic pain for many years. And so we used a novel, research-grade device connected to these electrodes that allowed not only stimulation of electricity but sensing. We could record electrical signals from the brain out in the real world.
So over many months, patients were asked to answer surveys related to the severity and the quality of their pain symptoms multiple times a day. What we did is we used just the brain signals in certain machine learning models to try to predict what these chronic pain score reports, the symptom or the patient provided.
We were essentially using brain activity as an input into a model to predict 0 to 10 scores, pain quality scores, and other aspects of the patient’s kind of lived experience that were reported to us.
CHARLES BERGQUIST: And did all four patients respond similarly?
PRASAD SHIRVALKAR: We actually found that there was one feature in common across all of patients that actually predicted high pain states in the real world. And that was actually a low frequency vibration signal in the orbitofrontal cortex.
CHARLES BERGQUIST: So even though these four patients have different experiences of pain, by looking for this low frequency signal in the specific part of the brain, you can tell, they are experiencing pain?
PRASAD SHIRVALKAR: That’s exactly right. So this low-frequency signal was the common signal across patients that actually seems to track when patients would enter a high-pain state.
CHARLES BERGQUIST: So you link the chronic pain experience to the specific brain part, the orbitofrontal cortex. Is that significant in some way? What else does that get involved with in the brain?
PRASAD SHIRVALKAR: So the orbitofrontal cortex was a pretty novel finding from this study because it’s not a brain region that’s typically associated with chronic pain. In fact, the most common functions that have been attributed to the orbitofrontal cortex are actually those important for decision making, knowing when a task or knowing when you need to shift your attention from one task to another.
And research from one of my mentor’s labs, Dr. Eddie Chang, showed that the orbitofrontal cortex actually harbors signals that allow us to predict whether a patient is going to be depressed or happy at any given time.
And so it’s interesting that this brain region that’s typically been associated with emotional regulation as well as decision making seems to play a huge role in chronic pain states.
CHARLES BERGQUIST: So you’ve found this common signal that could serve as some kind of biomarker of, these people are experiencing pain. Is there some way that you could short circuit it or preempt it somehow?
PRASAD SHIRVALKAR: That’s the goal. So as part of the larger clinical trial that these patients were in, our primary goal is to try to relieve their suffering. The biomarkers that we detected, they were kind of the first part of the study. And the goal is to take the individual biomarkers for each patient and integrate them into an algorithm that can provide personalized brain stimulation.
Hopefully, by using the biomarkers as a kind of sensing signal for their chronic pain state, we could decide when to turn the stimulator on and off. So I think of it as, we’re trying to build a thermostat to treat chronic pain where the individual biomarkers for each patient can be tuned such that the stimulator is providing therapy when that patient individually needs it.
CHARLES BERGQUIST: So I’d assume, A, it’s going to take a long time for any kind of brain-stimulating implant to be approved. And some people probably aren’t going to even want you to be sticking things in their head. Does this research point to any ways outside of a surgical treatment that could help people with chronic pain?
PRASAD SHIRVALKAR: Yes, yes, we would not want to insert electrodes into a patient’s brain unless it was really a therapy or an option of last resort, which is the case for the patients in this study. The signals we detected were using direct cortical recordings, right, so electrical signals directly from inside the brain, which is actually probably not feasible for treatment or diagnosis of the vast majority of people.
The fact that we detected signals directly inside the brain now gives us hope that we might be able to use certain non-invasive techniques to try to detect them, such as EEG, using near-infrared spectroscopy, or other kinds of sensors that obviously aren’t surgically implanted.
It remains to be seen. But I think this is going to be a really important obstacle that my lab is working on.
CHARLES BERGQUIST: How many people could this potentially help?
PRASAD SHIRVALKAR: Chronic pain is staggeringly common. There’s a new study published last week in JAMA that demonstrates that chronic pain is more common than depression, more common than diabetes, even more common than high blood pressure. One out of five people in the US suffers from chronic pain.
While the brain stimulation therapy that we use is reserved for the most severe refractory chronic pain cases, hopefully the results from this study are showing biomarkers where we can objectively track subjective states of chronic pain can be validated and generalized to a much larger population.
CHARLES BERGQUIST: Well, this is fascinating. Wishing you good luck with your future research. Dr. Prasad Shirvalkar is a neurologist and associate professor at the University of California San Francisco. Thanks so much for taking the time to talk with me today.
PRASAD SHIRVALKAR: Thank you I enjoyed our conversation.
Copyright © 2023 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Rasha Aridi is a producer for Science Friday and the inaugural Outrider/Burroughs Wellcome Fund Fellow. She loves stories about weird critters, science adventures, and the intersection of science and history.
As Science Friday’s director and senior producer, Charles Bergquist channels the chaos of a live production studio into something sounding like a radio program. Favorite topics include planetary sciences, chemistry, materials, and shiny things with blinking lights.