Subscribe to Science Friday
In September, an advisory committee for the Food and Drug Administration unanimously confirmed that phenylephrine—a common ingredient in cold medicines, including some types of Mucinex and Robitussin—doesn’t work.
For many physicians, pharmacists, and cold-sufferers, this came as no surprise. Phenylephrine’s ineffectiveness had been an open secret in the healthcare community for decades.
In 2005, Dr. Randy Hatton, clinical professor at the Pharmaceutical Outcomes and Policy Department at the University of Florida, managed the University of Florida Drug Information and Pharmacy Resource Center hotline. He often received calls from pharmacists reporting that phenylephrine-based drugs had no effect on improving colds.
He came across research from Dr. Leslie Hendeles, professor emeritus of the College of Pharmacy, also at the University of Florida, from a decade prior. Dr. Hendeles had also found that the substance was ineffective. They partnered up and petitioned the FDA to publicly confirm their finding. Their collaboration was the first step toward the FDA’s recent announcement.
But despite the announcement, the removal of these drugs from shelves is not guaranteed. Pharmaceutical companies are appealing the FDA’s decision, and are trying to stall an official declaration that prohibits their sale.
Guest host Flora Lichtman talks with Dr. Hatton and Dr. Hendeles about the long road to the FDA’s announcement. They discuss how their research proved phenylephrine’s ineffectiveness, and which drugs people can turn to instead as cold season approaches.
Further Reading
- Read coverage of CVS’s decision to pull certain cold medicines from its shelves via CNBC.
Segment Guests
Dr. Randy Hatton is a clinical professor of Pharmaceutical Outcomes & Policy at the University of Florida in Gainesville, Florida.
Dr. Leslie Hendeles is professor emeritus in the College of Pharmacy at the University of Florida in Gainesville, Florida.
Segment Transcript
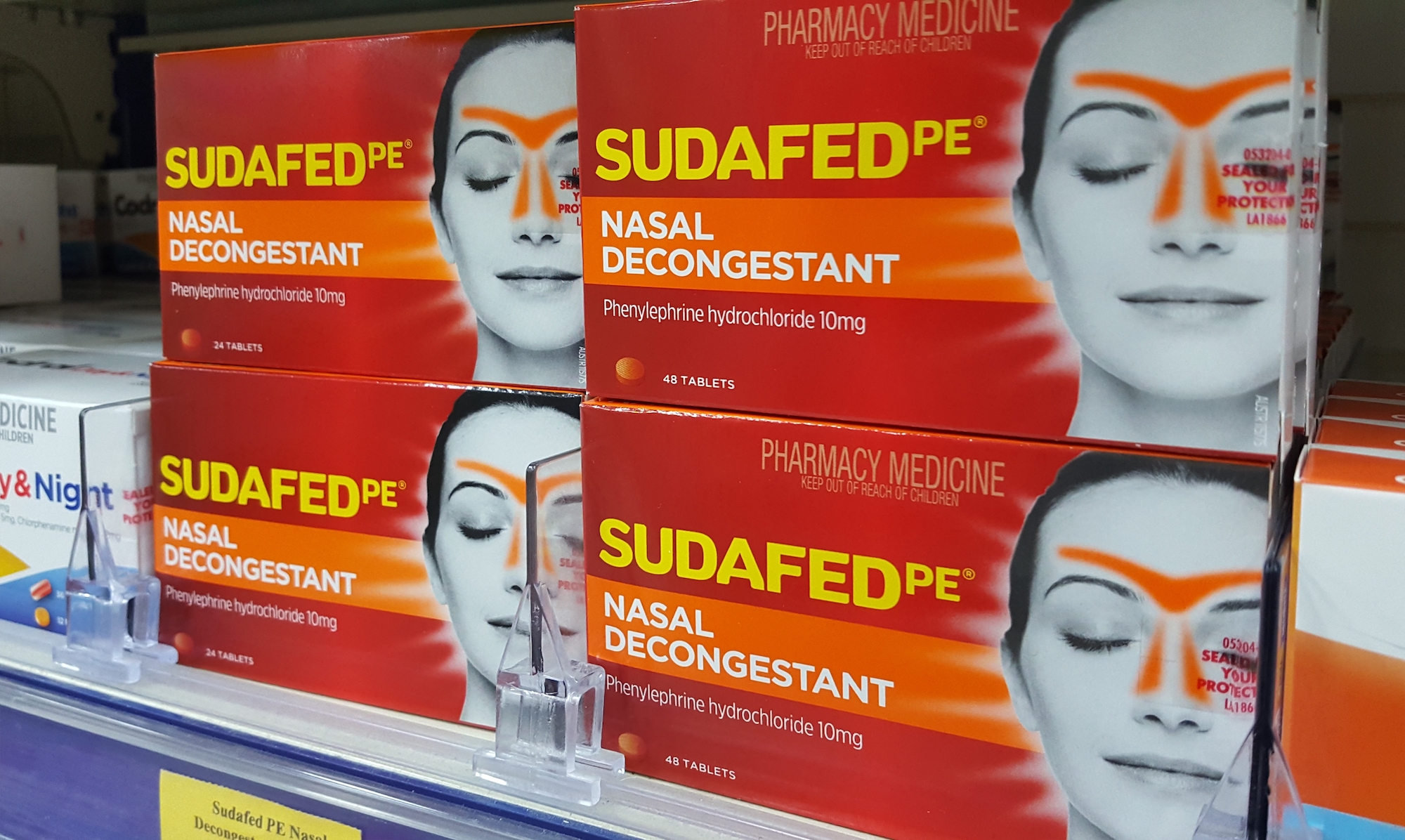
FLORA LICHTMAN: This is Science Friday. I’m Flora Lichtman. Big drama in the cold medicine world. You might have seen this story. A couple of months ago, an advisory committee for the Food and Drug Administration unanimously confirmed that a common ingredient in many cold medicines doesn’t work. The ingredient is called phenylephrine, and it’s found in hundreds of medicines, including some types of Sudafed and DayQuil.
Americans spent $1.8 billion on these sneeze oils last year. For many physicians and pharmacists, this finding came as no surprise. It was an open secret in the health care community for decades that oral phenylephrine doesn’t work. But for many cold sufferers, it was a blow.
Just last week, CVS pulled medicine with oral phenylephrine from their shelves based on the FDA’S announcement, but what happens next? I’m joined by two pharmacists who worked for decades to bring this to light Dr. Randy Hatton is a clinical professor at the University of Florida and Dr. Leslie Hendeles is a professor emeritus at the College of Pharmacy also at the University of Florida. Welcome to Science Friday.
RANDY HATTON: Thank you.
LESLIE HENDELES: Thank you.
FLORA LICHTMAN: OK, tell me about this debunked ingredient phenylephrine. When did it first appear in cold medicines, Randy?
RANDY HATTON: Well, it’s actually been first in cold medicines quite a very long time ago, all the way back in the 1930s. So it has been around a very long time. However, when it was first marketed, it was marketed as a nasal spray.
FLORA LICHTMAN: Not orally taken.
RANDY HATTON: No, it was about a decade later that it was marketed as an oral form.
FLORA LICHTMAN: So it’s been around for a long time, but am I right that this was an open secret that it didn’t work?
RANDY HATTON: Yes, that is the feedback we’ve gotten from many pharmacists and from some patients that they know that it doesn’t work.
FLORA LICHTMAN: Leslie, is this the kind of thing that you all discuss at pharmacist’s holiday parties?
LESLIE HENDELES: No, it’s been a conversation that’s occurred at continuing education meetings and from pharmacists just asking questions. Why did it get switched? And by the way, it’s not just cold products. It’s a huge number of allergy products, as well.
Stuffy nose can be caused by the common cold, or it can be caused by a seasonal allergy like ragweed during the August, September season. And nasal stuffiness can be a problem continuously. And it most often causes people to have difficulty sleeping.
FLORA LICHTMAN: Yeah, so people rely on these medicines that ultimately are doing nothing.
LESLIE HENDELES: Correct, but sometimes they might be taking a product. For example, in the case of allergies, they may be taking an antihistamine decongestant combination, and the antihistamine component still provides benefit for the runny nose, the red, watery, itchy eyes but not the nasal stuffiness. That’s why the decongestants combined in it. In those cases, the patient may get some symptom relief but not for the nasal stuffiness.
FLORA LICHTMAN: Randy, how did Operation Debunk Phenylephrine begin?
RANDY HATTON: Well, it began by getting calls to our statewide drug Information center at the University of Florida. After pseudoephedrine was moved behind the counter and manufacturers reformulated their products to substitute phenylephrine for pseudoephedrine in their oral decongestant products, pharmacists started calling the drug information center asking the question, does oral phenylephrine work, or what is the correct dose of oral phenylephrine?
Now, the drug information center is a teaching laboratory for doctor of pharmacy students at the time. And they would receive questions, formulate the question, research them, and then provide an answer back. As part of that search, we quickly came across Dr. Hendeles’ article from 1993, where he had reviewed oral decongestants and found that oral phenylephrine was ineffective.
Since we knew each other, offices were quite close together, we got together, started talking about this, and set out our quest to try to determine, at first, whether the evidence supported oral phenylephrine or not, and then follow on to try to take action, once we determined that we felt that the evidence was clear that it was ineffective.
FLORA LICHTMAN: Leslie, I want to come back to your scientific work in a minute, but just, Randy, why did pharmacists suspect it didn’t work? Why were they calling in the first place?
RANDY HATTON: The customers, the patients that they had, were complaining. They were used to taking products that had pseudoephedrine, which is quite effective when taken orally. And now, all of a sudden, they were getting products that were ineffective. They were complaining it didn’t work like their old pseudoephedrine products.
Now, this is confusing because, for example, common brand name of pseudoephedrine that used to be in front of the counter was Sudafed. This was rebranded as Sudafed PE, and most people aren’t really careful about what they grab off the counter. And so when they took that home, it didn’t work like the product that they had previously used.
FLORA LICHTMAN: Leslie, Let’s talk about the evidence. So how do you prove scientifically that this is ineffective?
LESLIE HENDELES: Well, there’s two parts to that. First is, you conduct studies. You select patients with either stuffiness from a cold or stuffiness from allergies, and in a double-blind manner, meaning that neither the patient nor the investigator knows which compound they’re getting, you give them the medication or a placebo and measure their nasal stuffiness on a scoring system.
Or what was done early on in this process, was to measure nasal-airway resistance. If you’re feeling a stuffy nose, air is not moving through your nose, and if you open it up, air begins to move. And you can measure the flow of air indirectly by a decrease in airway resistance.
One piece of this that will interest your audience from a scientific standpoint, is the answer as to why does phenylephrine not work when you swallow it, but it does work, very well, when you spray it in through the nose. The answer to the question, is that there is enzymes in the gut and in the liver, that inactivate the compound before it gets into the bloodstream. So it can’t get to the nose.
So you found scientifically that it wasn’t working well or it wasn’t working at all? Well, in the more modern studies, that have used good technique and good statistical analysis, it didn’t work differently from a placebo, in other words, a sugar pill.
FLORA LICHTMAN: OK, so it was a decade’s long saga to get the FDA on board. So let me just see if I can summarize. You have this data suggesting phenylephrine is not effective, and eventually, the FDA agrees to take a look. But after reviewing, the answer comes back no. There’s not enough data to say one way or another.
So then more modern studies happen. You do a FOIA request for unpublished studies. The drug company, Schering-Plow runs a study where they gave oral doses of 4 times the usual dose found in medicine, and they find no effect. Then there’s another FDA advisory committee meeting, and finally, they agree this ingredient doesn’t do anything. And then just last week, CVS says it’s pulling these drugs, which seems like a big deal. But is the FDA going to say drug makers, you can’t use this anymore?
LESLIE HENDELES: Well, they haven’t reached a decision yet, but I can’t see how they can say anything different when their own advisory committee voted 16 to 0 that it doesn’t have any efficacy different from a placebo. I think there’s been a lot of pressure on the agency from the Consumer Health Care Product Association. And I think there’s some political issues there.
But I think ultimately, they will probably take some action. And I think that the oral form of phenylephrine will be removed. There are other medications over-the-counter currently that are very effective. And so if it’s removed, it’s not going to deprive a patient of having a treatment.
FLORA LICHTMAN: What should I be taking?
LESLIE HENDELES: Well, it depends on whether you have a cold or whether you have an allergy. If you have an allergy, there is a topical nasal steroid like Flonase or Nasacort that’s extremely effective. And it’s taken during the entire season that you have symptoms, and it is like a silver bullet.
If you have a cold, you can spray phenylephrine into your nose or one of the longer acting forms like Afrin works exactly the same as phenylephrine in the nose, but it has a longer duration of action.
FLORA LICHTMAN: Randy, it seems like this process has taken a long time. Is that frustrating?
RANDY HATTON: Yeah, you can’t help but be frustrated, but it was a long process. Even now that there’s been this advisory committee meeting where they voted unanimously that it was ineffective, it’ll still be drawn out. The FDA has a period of time where they can make a tentative final decision.
There is no guidelines for how long that could be. That could be quite a long period of time. Then they open it up for public comment. That is usually around three months, but it can be extended if they think this is such an important issue that requires more.
Then they have a period of time of, usually around six months, where they will respond to those comments. And even at that point, should they decide that to make the final determination that oral phenylephrine is ineffective, they would give manufacturers some period of time to reformulate their products.
And that could be quite a period of time. There won’t be any recall because there is no safety issue because as Leslie mentioned, it’s not absorbed enough to be effective. It’s also not absorbed enough to be toxic.
FLORA LICHTMAN: You know, I wanted to know why you two made this your hill. This is a lot of work over many, many years. What compelled you both to do this?
RANDY HATTON: The compelling thing is to do the right thing. We felt the evidence was pretty clear that oral phenylephrine was ineffective. Yet, it’s on the market. Patients are spending their hard-earned money on these products. And we take a very evidence-based approach to the way we recommend drug therapies to patients.
So the evidence showed it didn’t work. So why should it be on the market? And further, a drug, whether it’s over the counter or it’s a prescription drug, not only has to be safe, it has to be effective. And oral phenylephrine is not effective.
LESLIE HENDELES: So I’ve been teaching pharmacists and physicians how to optimally use these medications for asthma and allergies for almost 50 years. It’s been my job to be on top of what’s effective and what’s not and to teach that information. So that’s been my motivation.
FLORA LICHTMAN: Well, I want to thank you both for doing this work. As a consumer and a frequent cold sufferer, I have two little kids, I am very grateful to you.
LESLIE HENDELES: Our pleasure.
RANDY HATTON: Thank you for your attention to this important issue. As Leslie said, getting the message out is part and teaching people is very important to us.
FLORA LICHTMAN: That was Dr. Randy Hatton, clinical professor at the University of Florida, and Dr. Leslie Hendeles, professor emeritus also at the University of Florida.
Copyright © 2023 Science Friday Initiative. All rights reserved. Science Friday transcripts are produced on a tight deadline by 3Play Media. Fidelity to the original aired/published audio or video file might vary, and text might be updated or amended in the future. For the authoritative record of Science Friday’s programming, please visit the original aired/published recording. For terms of use and more information, visit our policies pages at http://www.sciencefriday.com/about/policies/
Meet the Producers and Host
About Dee Peterschmidt
Dee Peterschmidt is a producer, host of the podcast Universe of Art, and composes music for Science Friday’s podcasts. Their D&D character is a clumsy bard named Chip Chap Chopman.
About Charles Bergquist
As Science Friday’s director and senior producer, Charles Bergquist channels the chaos of a live production studio into something sounding like a radio program. Favorite topics include planetary sciences, chemistry, materials, and shiny things with blinking lights.
About Flora Lichtman
Flora Lichtman is a host of Science Friday. In a previous life, she lived on a research ship where apertivi were served on the top deck, hoisted there via pulley by the ship’s chef.